
When your child gets a bad ear infection or you develop a urinary tract infection, you expect a simple prescription to fix it. But in 2026, that’s no longer guaranteed. Antibiotic shortages are no longer rare headlines-they’re daily realities in hospitals, clinics, and pharmacies across the UK, the US, and beyond. And the consequences aren’t just inconvenient. They’re deadly.
Why Antibiotics Are Disappearing
Antibiotics are different from other drugs. You don’t take them for years like blood pressure medicine. You take them for a week, then stop. That makes them low-profit products. Manufacturers don’t make much money off them, but they still need expensive, sterile factories to produce them. When the price of penicillin drops 27% over a decade, and compliance costs rise 34%, companies walk away. India and China dominate production, but supply chains are fragile. Brexit alone pushed UK antibiotic shortages from 648 in 2020 to over 1,600 in 2023. The European Court of Auditors called it a failure of oversight-no one was forcing manufacturers to invest in reliable production lines.The Global Crisis in Numbers
As of late 2024, 147 antibiotic shortages were active in the US alone, according to the FDA. Globally, 37 antimicrobials were officially listed as in short supply. The European Economic Area reported 28 countries facing shortages, with 14 calling them critical. In the UK, amoxicillin-a basic, cheap antibiotic used for everything from ear infections to pneumonia-has been rationed since early 2023. Hospitals had to cut its use by over 60% in some areas. That’s not a minor adjustment. It’s a system failure.What Happens When Antibiotics Vanish
When penicillin G benzathine isn’t available, doctors can’t treat syphilis properly. When amoxicillin runs out, they turn to stronger drugs like amoxicillin-clavulanate, which pushes bacteria to evolve faster. When those run out too, clinicians are forced to use last-resort antibiotics like colistin-a toxic drug that can damage kidneys and nerves. One infectious disease specialist in California told the APHA forum she had to give colistin to a healthy woman with a routine UTI. She was 28. She didn’t need it. But there was no other option. In low-income countries, the situation is worse. In rural Kenya, nurses report sending patients home without treatment because penicillin simply isn’t in stock. In Mumbai, a mother waited 72 hours for azithromycin to treat her child’s pneumonia. By the time it arrived, the infection had worsened. The child ended up in intensive care. These aren’t outliers. They’re symptoms of a broken system.Resistance Is Rising Because of Shortages
This isn’t just about running out of pills. It’s about what happens when you replace one antibiotic with another. When third-generation cephalosporins disappear-drugs that used to treat most E. coli and K. pneumoniae infections-doctors have no choice but to use carbapenems. These are broad-spectrum antibiotics, often reserved for the most dangerous infections. But when you use them for simple cases, you create superbugs. The WHO’s 2025 report found that resistance has increased in over 40% of pathogen-antibiotic combinations since 2018. One in six bacterial infections worldwide is now resistant. In urinary tract infections, it’s one in three.How Hospitals Are Trying to Cope
Hospitals are scrambling. Some set up antibiotic stewardship programs-teams that track usage, push for faster diagnostics, and avoid unnecessary prescriptions. Johns Hopkins reduced broad-spectrum antibiotic use by 37% during shortages by using rapid tests to identify infections within hours. But only 37% of US hospitals meet all WHO standards for these programs. In the UK, pharmacists are spending 22% more time managing shortages. Rationing decisions are now part of daily work. One NHS pharmacist in Birmingham said, “We’re playing Russian roulette with antibiotics. We give the strongest one first, hoping it lasts, but we know we’re making resistance worse.”Why Importing Doesn’t Fix It
High-income countries try to import antibiotics from other regions. But that’s not a solution-it’s a bandage. The global supply chain is stretched thin. When India faces a monsoon or China shuts down a factory for inspections, shortages ripple worldwide. The US FDA approved two new manufacturing facilities in January 2025, which should ease 15% of current shortages by late 2025. But building new plants takes years. And even if they’re built, will they be profitable? The market for generic antibiotics grew just 1.2% from 2019 to 2024. The rest of the pharmaceutical industry grew over 5%. Why would any company invest here?
The Human Cost
The Review on Antimicrobial Resistance predicts that without major change, antibiotic shortages will cause 1.2 million extra deaths annually by 2030. That’s not a future prediction. It’s a projection based on today’s trends. These aren’t abstract numbers. They’re mothers, children, elderly patients, cancer survivors recovering from chemo-all vulnerable to infections that used to be easily treatable. In 2023, a patient in Birmingham died from a simple skin infection. The hospital had run out of flucloxacillin. The next available option was delayed by five days. By then, the infection had spread to the bloodstream.What’s Being Done-And What’s Not
The WHO launched a $500 million Global Antibiotic Supply Security Initiative in late 2025, backed by G7 nations. The European Commission is pushing new rules to guarantee minimum stockpiles. But these are long-term plans. The immediate problem? No one is paying manufacturers enough to make the drugs. The WHO wants 70% of antibiotic use to come from the safest, narrowest-spectrum drugs by 2030. Right now, it’s only 58%. And the global market for antibiotics is smaller than it was a decade ago. Without financial incentives, manufacturers won’t change.What You Can Do
You can’t fix the supply chain. But you can help stop the crisis from getting worse. Don’t demand antibiotics for colds or flu-they don’t work. Finish your full course, even if you feel better. Don’t save leftover pills for next time. Ask your doctor if there’s an alternative. Support policies that fund antibiotic production. And if you’re a healthcare worker, push for better stewardship programs. This isn’t just about pills. It’s about preserving the ability to treat infections at all.Why are antibiotic shortages worse than other drug shortages?
Antibiotics are different because they’re often the only effective treatment for bacterial infections. Unlike painkillers or blood pressure meds, there aren’t always alternatives. If you run out of insulin, you can use another type. If you run out of penicillin for strep throat, you might have to use a stronger, riskier drug-or nothing at all. Plus, misuse during shortages accelerates resistance, making future infections harder to treat.
Is this problem only in the UK and US?
No. Antibiotic shortages are global. The WHO’s 2025 report shows the worst impacts are in South-East Asia and the Eastern Mediterranean, where one in three infections is resistant. Low- and middle-income countries face even greater challenges-70% of antibiotics are already inaccessible there. Even countries with strong healthcare systems, like Germany and Canada, are seeing critical shortages of key drugs like amoxicillin and ceftriaxone.
Can I buy antibiotics online to avoid shortages?
Never. Online pharmacies selling antibiotics without prescriptions are illegal and dangerous. You might get fake, expired, or wrong-dose pills. Worse, you might take the wrong antibiotic for your infection, which can worsen resistance. Always get antibiotics through a licensed healthcare provider who can diagnose properly and choose the right drug.
Are new antibiotics being developed?
Very few. Drug companies focus on chronic diseases because they’re more profitable. Only 22% of new antibiotic candidates in development target the most dangerous resistant bacteria. Even when new ones are approved, it takes years to scale up production. The pipeline is thin, and manufacturing isn’t keeping pace.
How long will this shortage last?
There’s no end in sight unless governments and manufacturers act. The WHO projects shortages will increase by 40% by 2030. New manufacturing facilities may help in the next 2-3 years, but without financial incentives-like guaranteed minimum prices or government contracts-companies won’t stay in the market. This isn’t a temporary hiccup. It’s a systemic collapse.
11 Comments
Write a comment
More Articles

How to Buy Cheap Generic Lasix Online Safely
Learn how to safely purchase cheap generic Lasix online, verify prescriptions, compare accredited pharmacies, and save money while staying compliant.
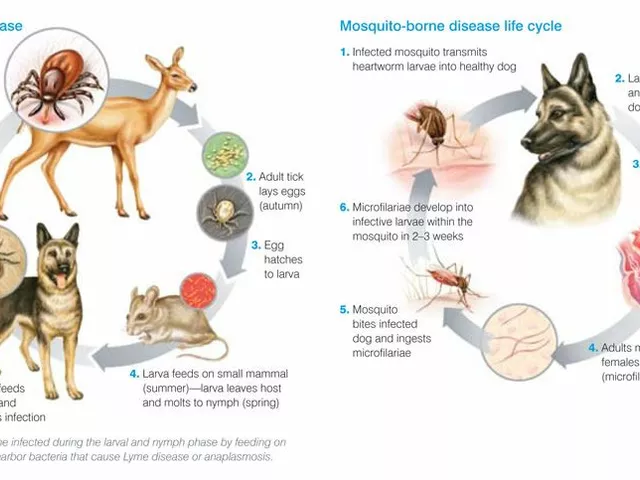
Tick Fever: What You Need to Know About This Dangerous Disease
Tick Fever, also known as Tick-Borne Disease, is a serious illness transmitted by ticks. It's crucial to be aware that this disease can have severe health implications including fever, headache, and fatigue, and in some cases can even be fatal. Early detection and treatment are absolutely vital. It's also important to take steps in preventing tick bites, such as using repellents and wearing appropriate clothing when in tick-infested areas. Stay safe out there, folks!

Roisin Kelly
January 20, 2026 AT 16:46This is all just a big pharma scam to make us buy more expensive drugs-why do you think they let antibiotics get so cheap? They knew people would panic when they ran out and then pay ten times more for the ‘new miracle drug’ they’re secretly developing.