When dentists look for a drug that can calm nerves, reduce bleeding, and keep pain at bay, they often turn to familiar agents like lidocaine or midazolam. Clonidine is a selective α2‑adrenergic agonist originally approved for hypertension that has found a niche in oral surgery because of its unique blend of analgesic, anxiolytic, and vasoconstrictive effects.
Key Takeaways
- Clonidine can be used as an adjunct to local anesthetic to improve pain control and reduce intra‑operative bleeding.
- Its sedative properties help anxious patients stay calm without deep sedation.
- Typical oral doses are low (0.1‑0.2 mg) and can be administered orally, intravenously, or as a transdermal patch.
- Side‑effects include dry mouth, hypotension, and bradycardia, so monitoring is essential.
- When combined with conventional anesthetics, clonidine shortens postoperative analgesic requirements.
How Clonidine Works in the Mouth
The drug binds to presynaptic α2 receptors in the sympathetic nervous system, inhibiting norepinephrine release. This dampens the body’s “fight‑or‑flight” response, producing two clinically useful effects for dentistry:
- Analgesia: reduced transmission of pain signals at the spinal cord level.
- Vasoconstriction: narrowed blood vessels lower bleeding during surgery.
Because it works centrally as well as peripherally, clonidine adds a layer of comfort that typical local anesthetics alone cannot provide.
Clinical Uses of Clonidine in Dental Settings
Dental professionals have reported success with clonidine in several scenarios. Below are the most common:
- Periodontal surgery: reduced intra‑operative bleeding improves visibility.
- Dental implant placement: enhanced analgesia shortens the need for postoperative opioids.
- Extraction of impacted teeth: especially in patients with high anxiety.
- Root canal therapy: adjunctive analgesia helps patients tolerate longer appointments.
- Oral pathology biopsies: better hemostasis when large vascular lesions are involved.
In each case, clonidine is typically given as a pre‑medication (oral or buccal) 30‑45 minutes before the procedure, or intravenously right before local anesthetic injection.

Benefits Over Traditional Sedatives and Vasoconstrictors
While benzodiazepines and epinephrine‑containing anesthetics are standard, clonidine offers a distinct profile:
| Feature | Clonidine | Midazolam | Epinephrine (in LA) |
|---|---|---|---|
| Primary action | α2‑adrenergic agonist (analgesic + sedative) | GABA‑modulator (sedative) | Vasoconstrictor |
| Onset | 30‑45 min (oral) | 2‑5 min (IV) | Immediate (local) |
| Duration | 4‑6 h | 1‑2 h | As long as LA lasts |
| Bleeding control | Yes (via vasoconstriction) | No | Yes (local only) |
| Post‑op opioid need | Reduced by ~30% | Little impact | Minimal impact |
| Side‑effects | Dry mouth, hypotension, bradycardia | Respiratory depression, amnesia | Hypertension, tachycardia |
For patients who need both sedation and hemostasis without the cardiac spikes linked to epinephrine, Clonidine dentistry becomes a compelling option.
Dosage, Administration Routes, and Safety Considerations
Dental protocols vary, but the most widely cited regimens come from oral surgery literature:
- Oral pre‑medication: 0.1 mg (1 µg/kg) to 0.2 mg taken 30 minutes before the procedure.
- Intravenous bolus: 1‑2 µg/kg administered slowly over 2 minutes, followed by a maintenance infusion of 0.5‑1 µg/kg/min if prolonged sedation is needed.
- Transdermal patch: 0.1 mg/24 h applied the night before; rarely used in dental clinics due to onset time.
Because clonidine lowers blood pressure, it’s essential to measure baseline vitals and watch for a drop of more than 20 mmHg systolic. Patients with pre‑existing hypotension, severe bradycardia, or heart block should be excluded.

Potential Side Effects and Contra‑indications
Most adverse events are mild and dose‑related. Commonly reported issues include:
- Dry mouth (xerostomia)
- Light‑headedness or dizziness
- Transient hypotension
- Bradycardia (especially in elderly patients)
Rare but serious reactions-such as severe heart block or rebound hypertension after abrupt discontinuation-warrant immediate medical attention. Clonidine is contraindicated in patients with:
- Uncontrolled hypertension
- Severe cardiac conduction disorders
- Known hypersensitivity to α2‑adrenergic agonists
- Pregnancy (category C) unless benefits outweigh risks
Practical Tips for Dental Professionals
Integrating clonidine into a practice doesn’t require major changes, but a few best‑practice steps smooth the process:
- Screen patients thoroughly: Use a short questionnaire to flag cardiovascular issues.
- Standardize the pre‑med protocol: Keep oral tablets in a locked drawer, label with dose, and record administration time.
- Monitor vitals: Check blood pressure and heart rate before, during, and after the procedure.
- Educate the team: Ensure assistants know the signs of excessive hypotension and can raise the head of the chair quickly.
- Document outcomes: Track postoperative pain scores and any side‑effects; over time this data helps refine dosing.
When used responsibly, clonidine can reduce the need for opioids, shorten recovery time, and improve patient satisfaction-key metrics for any modern dental practice.
Frequently Asked Questions
Can clonidine replace lidocaine?
No. Clonidine is an adjunct, not a substitute. It enhances analgesia and reduces bleeding but does not provide the rapid numbness that lidocaine offers.
How long before a procedure should a patient take oral clonidine?
Typically 30‑45 minutes. This allows plasma levels to peak and the sedative effect to settle.
Is clonidine safe for children undergoing dental extractions?
Pediatric use is off‑label and should be approached with caution. Dosing is weight‑based (0.05‑0.1 mg) and requires close monitoring by a pediatric anesthesiologist.
What should I do if a patient becomes hypotensive after clonidine?
Raise the chair, administer a slow IV bolus of normal saline, and if needed, give a small dose of a vasopressor such as phenylephrine under medical supervision.
Can clonidine be combined with other sedatives?
Yes, but the total sedation load must be calculated. Low‑dose midazolam plus clonidine can produce synergistic anxiolysis while allowing lower doses of each drug.
With a clear understanding of its pharmacology, dosing, and safety profile, dentists can confidently add clonidine to their armamentarium and deliver smoother, less painful procedures for patients who need it most.
8 Comments
Write a comment
More Articles

Unlock Nature’s Healing: Oregon Fir Balsam Supplement Benefits & Guide
Dive into the world of Oregon Fir Balsam and discover its unique place in the natural supplement scene. This article explores the science, uses, and real-world experiences surrounding fir balsam extract. Expect to learn surprising facts, practical wellness tips, and how this forest-sourced remedy could fit into your routine. If you're curious about the power of conifers in your health journey, this is for you.

How to Read Interaction Warnings on Medication Guides
Learn how to read interaction warnings on medication guides to avoid dangerous drug combinations. Understand severity levels, hidden risks from OTC meds and supplements, and practical steps to stay safe.
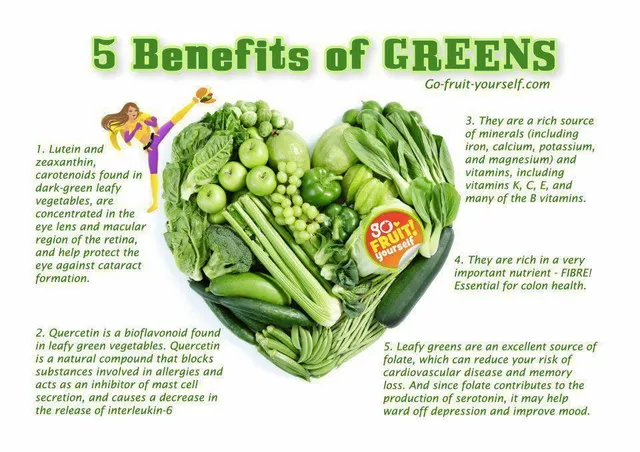
Folate Deficiency and Eye Health: What You Need to Know
As a blogger, I recently came across an important topic concerning eye health - folate deficiency. Folate, also known as vitamin B9, plays a crucial role in maintaining our overall well-being, including our precious eyesight. A deficiency in folate can lead to various eye problems, such as macular degeneration and optic neuropathy. To prevent these issues, it's essential to consume a balanced diet rich in leafy greens, beans, and fortified cereals. So, let's take care of our eyes by ensuring we get enough folate in our daily diets!
asha aurell
October 26, 2025 AT 16:51Clonidine’s benefits are overrated; the evidence for reduced bleeding is minimal. Most dentists would be better off sticking to proven vasoconstrictors.