Understanding Diabetic Gastroparesis
Before diving into ways to cope with diabetic gastroparesis, it's essential to understand what it is and why it occurs. Diabetic gastroparesis is a condition in which the stomach takes too long to empty its contents, primarily due to nerve damage caused by high blood sugar levels in people with diabetes. This slow emptying can lead to nausea, vomiting, and other uncomfortable symptoms. In this article, we'll discuss some practical ways to manage these symptoms and improve your quality of life.
1. Consult Your Healthcare Team
As with any health concern, your healthcare team should be your first point of contact when dealing with diabetic gastroparesis. They can help you understand the condition, provide guidance on medication and treatment options, and monitor your progress. It's crucial to keep your healthcare team informed of your symptoms, as they can make adjustments to your treatment plan as needed.
2. Adjust Your Diet
One of the most significant ways to cope with nausea and vomiting related to diabetic gastroparesis is by making adjustments to your diet. Eating smaller, more frequent meals throughout the day can help reduce the amount of food in your stomach at any given time, which may alleviate symptoms. You may also want to avoid high-fat and high-fiber foods, as they can slow down digestion even further. Consult with a registered dietitian to help create a meal plan that works best for you.
3. Stay Hydrated
Staying hydrated is crucial for overall health, but it can be especially important when dealing with diabetic gastroparesis. Dehydration can worsen nausea and vomiting, so be sure to drink plenty of water throughout the day. If you're struggling to keep fluids down, try sipping on small amounts of water or clear liquids like broth or electrolyte beverages.
4. Medication Management
There are several medications available that can help manage the symptoms of diabetic gastroparesis, such as medications to stimulate gastric emptying or to reduce nausea and vomiting. Speak with your healthcare provider about which medications might be right for you and be sure to take them as prescribed. Remember that it may take some trial and error to find the right medication and dosage for your symptoms.
5. Try Alternative Therapies
Some people find relief from nausea and vomiting related to diabetic gastroparesis through alternative therapies, such as acupuncture or ginger supplements. While these therapies may not work for everyone, they may be worth exploring if you're struggling to manage your symptoms with traditional treatment options. Be sure to discuss any alternative therapies with your healthcare provider before trying them.
6. Keep a Symptom Journal
Keeping a symptom journal can be a helpful tool in managing diabetic gastroparesis. By tracking your symptoms, you can identify patterns and triggers that may be contributing to your nausea and vomiting. This information can be helpful in making adjustments to your diet and treatment plan, as well as providing valuable insight to your healthcare team.
7. Manage Stress
Stress can worsen symptoms of diabetic gastroparesis, so finding ways to manage stress in your daily life is essential. Consider incorporating relaxation techniques, such as deep breathing exercises, meditation, or yoga, into your routine. Additionally, making time for hobbies and activities that bring you joy can help reduce stress and improve your overall well-being.
8. Get Support
Dealing with diabetic gastroparesis can be challenging, both physically and emotionally. It's essential to have a strong support system in place to help you manage your symptoms and cope with the emotional toll the condition can take. Reach out to friends and family for support, and consider joining a support group for people with diabetes or gastroparesis to connect with others who understand what you're going through.
9. Be Patient with Yourself
Managing diabetic gastroparesis is not a one-size-fits-all approach, and it may take some time to find the right combination of treatments and lifestyle adjustments that work for you. Be patient with yourself during this process, and remember that you're not alone in your journey. With the right support and resources, you can find ways to cope with the nausea and vomiting associated with diabetic gastroparesis and improve your quality of life.
10. Stay Informed
Lastly, staying informed about diabetic gastroparesis and its management is key to coping with the condition. Regularly communicate with your healthcare team, and stay updated on the latest research, treatment options, and resources available to you. The more you know about diabetic gastroparesis, the better prepared you'll be to manage your symptoms and maintain your quality of life.
18 Comments
Write a comment
More Articles

Minoxytop vs Other Hair‑Loss Treatments: Pros, Cons & Best Picks
A side‑by‑side review of Minoxytop vs finasteride, PRP, laser therapy, transplants and natural options, with a comparison table, tips and FAQs.
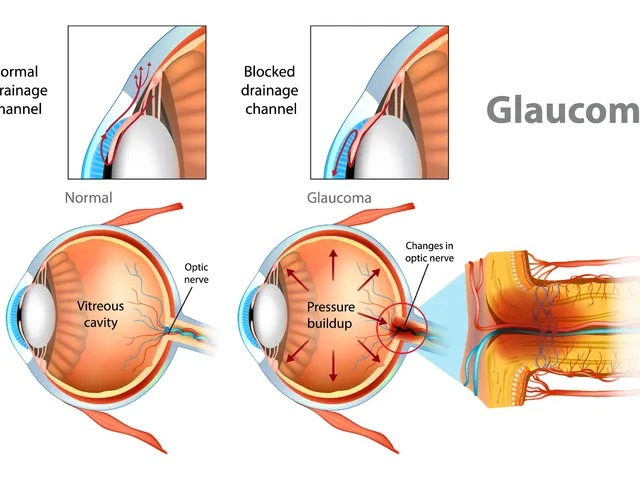
The effectiveness of dorzolamide in treating different types of glaucoma
Hey there, gentlemen! I just wanted to share some insights on a very interesting topic - the effectiveness of dorzolamide in treating different types of glaucoma. We'll dive into its mechanism of action, its beneficial effects on different types of this eye condition, and why it's becoming a go-to medication. Through this, I hope to provide everyone with a deeper understanding of this treatment option in a clear and simple language. Remember, knowledge is your best ally in health matters!

Military Deployment and Medication Safety: How Heat, Storage, and Access Impact Soldier Health
Military deployment exposes medications to extreme heat, storage failures, and access delays that can reduce vaccine potency by 50% and delay life-saving treatments. Learn how the military fights to keep meds effective-and what’s coming next.
Stephanie S
June 18, 2023 AT 22:37Great summary, and thanks for sharing! The tips about small, frequent meals, staying hydrated, and tracking symptoms are especially useful, and they really help to manage the nausea and vomiting associated with diabetic gastroparesis. It's also vital to keep your healthcare team in the loop, because they can adjust medications as needed, and they can provide referrals to dietitians and other specialists. Remember, patience and consistency are key, so keep at it!