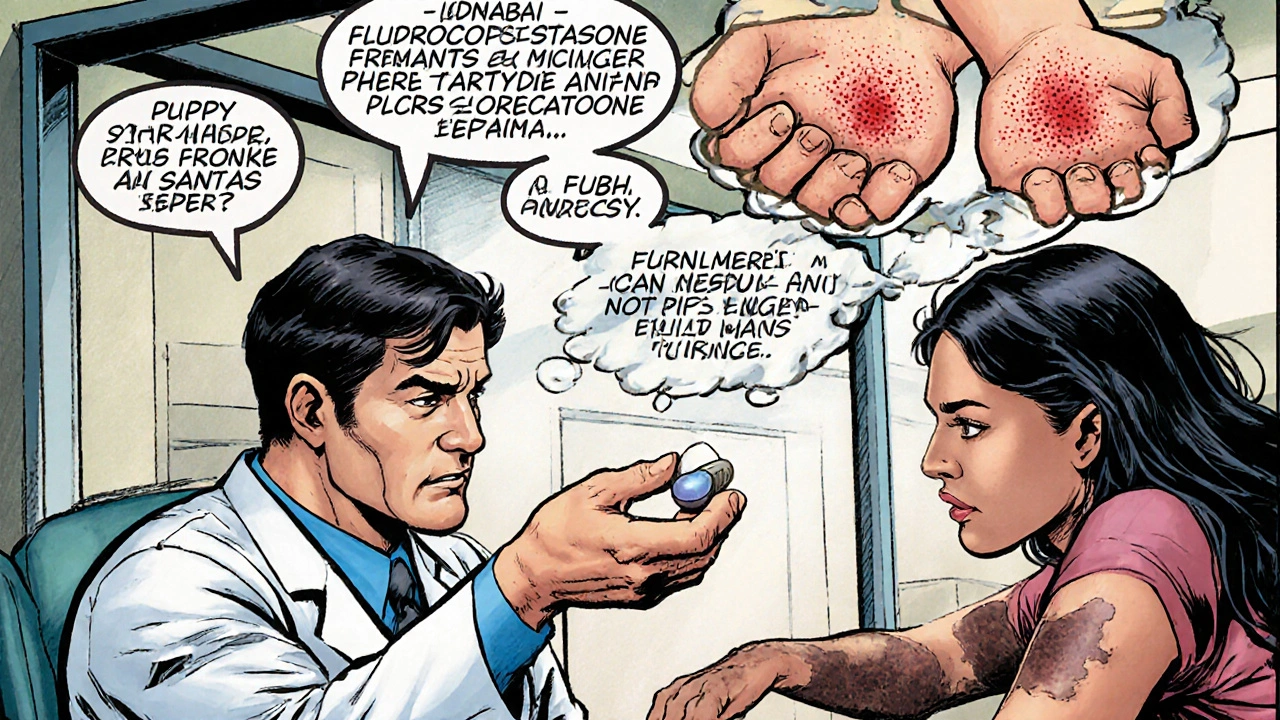
Fludrocortisone Skin Side Effects Tracker
Symptom Tracker
Fludrocortisone is commonly prescribed to treat adrenal insufficiency and certain blood‑pressure disorders, but many patients wonder how the drug might affect their skin. Below you’ll find a practical breakdown of the most frequently reported dermatological reactions, why they happen, and what you can do to keep your skin looking and feeling its best while on therapy.
Key Takeaways
- Fludrocortisone can cause skin‑related side effects such as edema, acne‑like eruptions, hyperpigmentation, and thinning.
- Most reactions are dose‑dependent and often improve when the dose is adjusted.
- Using a gentle skincare routine and monitoring changes early can prevent complications.
- Seek medical attention if you notice painful rashes, rapid skin darkening, or severe swelling.
- A simple checklist can help you track symptoms and communicate effectively with your doctor.
What Is Fludrocortisone?
Fludrocortisone is a synthetic mineralocorticoid medication that mimics the action of the natural hormone aldosterone. It helps the kidneys retain sodium and excrete potassium, thereby raising blood volume and blood pressure. It is FDA‑approved for primary adrenal insufficiency (Addison’s disease) and certain forms of orthostatic hypotension. The drug is usually taken once daily, with doses ranging from 0.05mg to 0.2mg depending on the condition being treated.
Why Skin Gets Involved
Although fludrocortisone primarily targets the kidneys, its mineralocorticoid activity reverberates throughout the body. The skin is a highly vascular organ, and changes in fluid balance or hormone levels can manifest there. Three main mechanisms explain the dermatological side effects:
- Fluid Retention: Excess sodium leads to water retention, which can cause swelling (edema) in the hands, feet, and lower legs.
- Hormonal Influence: Mineralocorticoids interact with skin receptors, potentially increasing sebum production and altering pigmentation.
- Immune Modulation: Corticosteroid‑like effects can thin the epidermis, making the skin more vulnerable to irritants and infections.
Common Skin‑Related Side Effects
Below is a quick snapshot of the side effects that patients report most often. Frequency data come from post‑marketing surveillance studies covering over 12,000 users worldwide.
| Side Effect | Typical Frequency | Typical Onset | Management Tips |
|---|---|---|---|
| Peripheral edema | Common (≈15‑20%) | 1‑4 weeks | Elevate legs, moderate sodium intake, discuss dose reduction with doctor. |
| Acne‑like papules | Uncommon (≈5‑8%) | 2‑6 weeks | Gentle cleanser, non‑comedogenic moisturizers, topical retinoid if needed. |
| Hyperpigmentation | Rare (<2%) | 1‑3 months | Sun protection, avoid irritants, consider topical hydroquinone under supervision. |
| Skin thinning / easy bruising | Rare (<1%) | 3‑6 months | Use mild soaps, avoid aggressive scrubbing, monitor for signs of infection. |
| Pruritus (itching) | Uncommon (≈4‑6%) | Variable | Moisturize regularly, consider antihistamine at night. |
Deep Dive: Hyperpigmentation and Its Triggers
Hyperpigmentation is one of the more striking, though still rare, skin changes linked to fludrocortisone. The drug can stimulate melanocytes indirectly by increasing circulating aldosterone‑like activity, which in turn raises cortisol levels slightly. In patients with darker baseline skin tones, even a subtle increase in melanin production can become noticeable.
Key risk factors include:
- High cumulative dose (>0.5mg per day over several months)
- Concurrent use of photosensitizing agents (e.g., certain antibiotics)
- Excessive sun exposure without protection
Management focuses on prevention: apply broad‑spectrum SPF30+ daily, wear protective clothing, and limit peak‑hour sun exposure. If dark patches appear, a dermatologist may prescribe a short course of topical azelaic acid or a low‑strength hydroquinone cream.
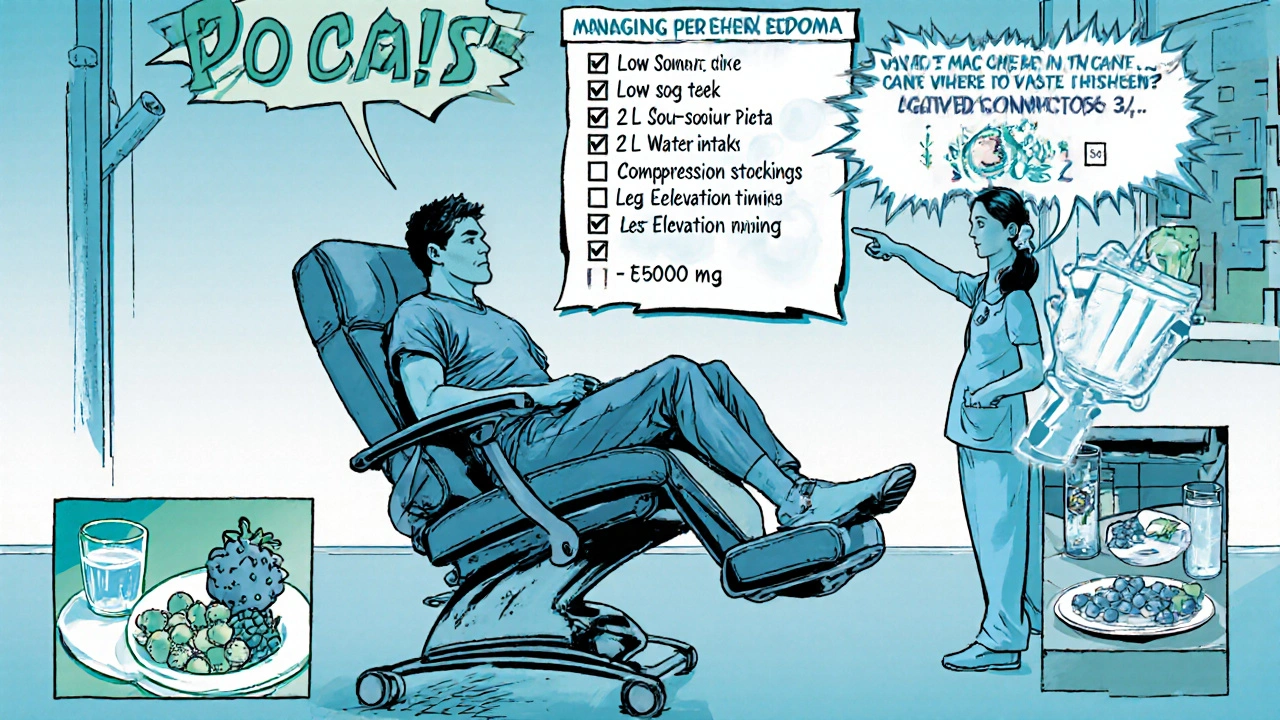
Peripheral Edema: When Swelling Becomes a Problem
Because fludrocortisone encourages the kidneys to hold onto sodium, fluid can leak into interstitial spaces, especially in the lower extremities. Most patients notice a mild puffiness that resolves with simple measures, but a small subset experiences painful, deep swelling that interferes with walking.
Practical steps to keep edema in check:
- Reduce sodium intake to 1500mg per day - think fresh fruits, vegetables, and unsalted nuts.
- Drink at least 1.5‑2L of water daily; proper hydration actually helps flush excess sodium.
- Elevate legs above heart level for 15‑20 minutes after long periods of sitting.
- Wear compression stockings (15‑20mmHg) if swelling persists.
- Schedule a follow‑up visit within 4‑6 weeks of starting therapy to assess whether the dose can be lowered.
Acne‑Like Breakouts and Sebum Production
Although fludrocortisone isn’t a classic anabolic steroid, its mineralocorticoid activity can still tip the balance of skin oils. In teenagers and young adults, even a modest increase in sebum may trigger acneiform eruptions on the forehead, cheeks, and upper back.
Effective strategies include:
- Cleanse twice daily with a mild, sulfate‑free formulation.
- Apply a non‑comedogenic moisturizer to avoid barrier disruption.
- Consider a topical benzoyl peroxide or clindamycin gel if lesions are inflammatory.
- Avoid heavy makeup or occlusive sunscreens; opt for mineral‑based SPF instead.
Skin Thinning and Easy Bruising
Long‑term exposure to any corticosteroid‑type molecule can compromise collagen synthesis. When skin becomes thinner, capillaries rupture more easily, leading to bruises that appear after minor bumps. Although this side effect is rare with fludrocortisone, patients on combined steroid regimens (e.g., oral prednisone plus fludrocortisone) should be vigilant.
Tips to protect fragile skin:
- Use lukewarm water rather than hot showers.
- Pat skin dry-don’t rub aggressively.
- Apply a barrier‑repair cream containing ceramides or niacinamide twice a day.
- Report any sudden increase in bruising to your clinician, especially if you’re also taking anticoagulants.
When to Seek Medical Attention
Most dermatological side effects are manageable with lifestyle tweaks, but some signals warrant a prompt call to your doctor:
- Rapid, painful swelling spreading beyond the ankles or hands.
- Sudden darkening of the face, neck, or inner elbows that doesn’t improve with sunscreen.
- Persistent, pus‑filled lesions that resist over‑the‑counter treatments.
- Severe itching accompanied by a rash that blisters or oozes.
Early intervention can prevent a minor irritation from becoming a full‑blown infection or a chronic skin condition.

Patient Self‑Monitoring Checklist
- Record any new skin changes in a daily journal (date, location, severity).
- Take photos of suspicious spots every week to track progression.
- Note your sodium intake and water consumption each day.
- Check your feet for swelling before bedtime; elevate if needed.
- Review the checklist with your prescriber at each follow‑up appointment.
How Doctors Adjust Treatment
Healthcare providers typically follow a stepwise approach:
- Confirm that the skin issue coincides with the start or dose increase of fludrocortisone.
- Rule out other causes (e.g., allergic reactions, infections, concurrent medications).
- If edema is prominent, consider reducing the dose by 0.025mg and re‑evaluate after two weeks.
- For acne‑like eruptions, add a topical agent rather than stopping fludrocortisone outright.
- In cases of severe hyperpigmentation or skin thinning, a short‑term switch to a lower‑potency mineralocorticoid may be recommended.
These adjustments aim to keep the primary therapeutic goal-stable blood pressure and electrolyte balance-while minimizing dermatological discomfort.
Mini FAQ
Can fludrocortisone cause allergic skin reactions?
True allergic reactions (e.g., urticaria, angioedema) are extremely rare. Most rashes are linked to fluid shifts or hormone‑driven changes rather than an immune‑mediated allergy. If you develop hives or swelling of the face and throat, treat it as an emergency and seek immediate care.
Is it safe to use over‑the‑counter acne treatments while on fludrocortisone?
Yes, most non‑prescription products (salicylic acid, benzoyl peroxide) are safe. Avoid potent cortisone creams unless a dermatologist specifically recommends them, as they could compound skin‑thinning effects.
How long does it take for edema to improve after dose reduction?
Most patients notice a reduction in swelling within 5‑10 days, though full resolution may take up to three weeks, especially if sodium intake remains high.
Should I stop fludrocortisone if I develop skin thinning?
Stopping abruptly can precipitate adrenal crisis, so never discontinue without medical guidance. Instead, discuss dose tapering or a switch to a milder mineralocorticoid with your doctor.
Are there any long‑term skin risks associated with chronic fludrocortisone use?
Long‑term data suggest that persistent high doses may increase the likelihood of chronic bruising and subtle skin atrophy. Regular dermatologic check‑ups and vigilant skin care can keep these issues manageable.
Next Steps for Patients
1. Review the self‑monitoring checklist and start a skin diary today.
2. Adjust your diet to stay under 1500mg of sodium per day.
3. Schedule a follow‑up appointment in 4‑6 weeks to discuss any skin changes you’ve logged.
4. If a new rash, swelling, or dark spot appears, contact your healthcare provider promptly-early tweaks are usually enough to keep you comfortable while staying protected by fludrocortisone.
By staying informed and proactive, you can enjoy the therapeutic benefits of fludrocortisone without letting skin side effects interrupt daily life.
17 Comments
Write a comment
More Articles

Rise of Next-Gen Viagra Alternatives in 2025: What You Need to Know
Curious about what's next after Viagra? This article digs into the 2025 wave of new alternatives, including advanced PDE5 inhibitors and innovative therapies shaking up erectile dysfunction treatment. Explore real results, learn what works, and get savvy about what's coming to pharmacy shelves soon. Whether you're after faster effects or fewer side effects, this guide helps you cut through the marketing and find the best science-backed options. Don't get stuck in the past; see how sexual health is evolving this year.

Antitrust Issues in Generic Substitution: How Big Pharma Blocks Cheaper Drugs
Big Pharma uses legal tricks like product hopping and REMS abuse to block generic drugs, keeping prices high. Learn how antitrust enforcement is fighting back-and why it matters for your wallet.
Telehealth Strategies for Monitoring Side Effects in Rural and Remote Patients
Telehealth is transforming how rural and remote patients manage medication side effects. From smart devices to pharmacist-led monitoring, discover how these strategies reduce hospitalizations and save lives in underserved areas.
Samantha Kolkowski
October 15, 2025 AT 13:29I’ve found that keeping sodium intake moderate really helps curb the peripheral edema that some folks experience on fludrocortisone. Pair it with an elevation routine for the legs and you’ll notice a reduction in swelling within a week or so. Also, choose a fragrance‑free moisturizer to combat the dryness that can come with skin thinning. And don’t forget to report any sudden darkening to your doctor – early detection is key.