When you're managing bipolar disorder with lithium carbonate, it's not just about taking a pill. The difference between feeling stable and slipping into depression or mania can come down to a tiny number: your serum lithium level. And if you're on a generic version, that number can shift unexpectedly-even if your doctor didn't change your dose.
Why Generic Lithium Isn't Always Interchangeable
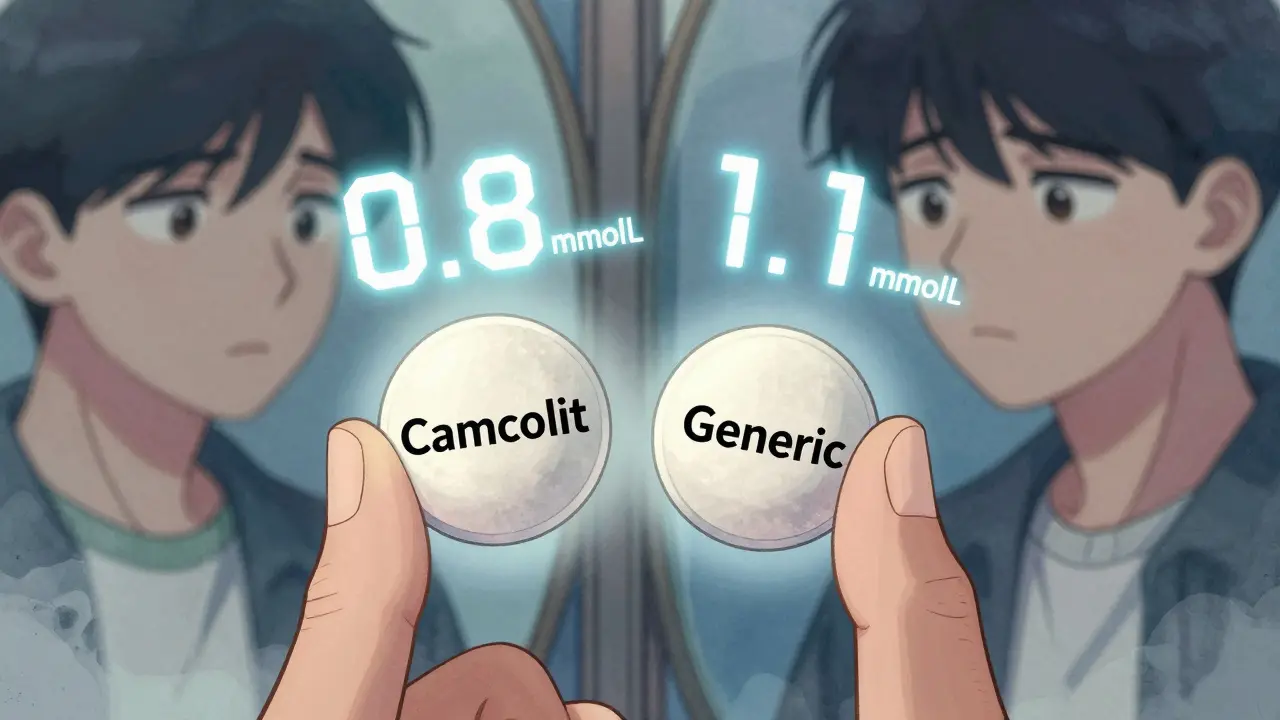
Lithium carbonate is one of the oldest and most effective mood stabilizers for bipolar disorder. But unlike many other medications, not all generic versions are created equal when it comes to how your body absorbs them. While the FDA requires generics to be bioequivalent to the brand-name drug, that doesn't mean they behave the same in your bloodstream. Take Camcolit and Priadel, two common sustained-release formulations. A 2024 study found that patients switched from one to the other ended up with 11% higher average serum lithium levels-even when the daily dose stayed the same. That might not sound like much, but in lithium therapy, even a 0.2 mmol/L change can push you from safe to toxic. Why does this happen? It’s all about how the tablet breaks down. Some generics release lithium slowly over hours. Others let it flood your system faster. Even small differences in coating, filler, or particle size change how quickly lithium enters your blood. For someone on a tight therapeutic window, that’s enough to cause side effects-or worse, trigger a relapse.The Narrow Window: What Your Serum Level Should Be
Lithium has one of the narrowest therapeutic indexes in all of medicine. That means the difference between a helpful dose and a dangerous one is razor-thin. For most adults, the target range is 0.6 to 1.2 mmol/L. But that’s not one-size-fits-all:- 0.6-0.8 mmol/L: Often used for long-term maintenance, especially in older adults or those with kidney issues.
- 0.8-1.0 mmol/L: Recommended for acute episodes or when symptoms are still present.
- Above 1.2 mmol/L: Risk of toxicity rises sharply. Levels over 1.5 mmol/L can cause tremors, confusion, and kidney damage. Above 2.0 mmol/L? That’s a medical emergency.
When and How to Check Your Levels
Getting your blood drawn at the wrong time can give you a false reading. Timing matters.- If you take lithium twice a day, your blood should be drawn 12 hours after your last dose. That’s when your level stabilizes.
- If you take it once daily (common with extended-release versions), the blood test should be done 24 hours after your last dose.

Who’s at Higher Risk?
Not everyone needs the same lithium level. Certain factors change how your body handles it:- Age over 60: Kidneys clear lithium slower. Many experts recommend lowering targets by 20-25% for older adults.
- Women: On average, women need lower doses than men-about 96 mg less per day-due to differences in body weight and fluid balance.
- People with kidney disease: Lithium is cleared by the kidneys. If your eGFR drops below 45 mL/min, your doctor should reduce your dose or consider alternatives.
- Those on diuretics or NSAIDs: Medications like ibuprofen, hydrochlorothiazide, or ACE inhibitors can cause lithium to build up dangerously. Always check with your doctor before starting any new drug.
What You Should Monitor Beyond Blood Levels
Lithium doesn’t just affect your brain. It impacts your whole body. Regular monitoring isn’t optional-it’s essential.- Thyroid function: Up to 15% of long-term users develop hypothyroidism. Get a TSH test every 6 months.
- Kidney function: Check serum creatinine and eGFR every 3-6 months. Some guidelines now recommend adding cystatin C for more accurate kidney assessment.
- Electrolytes: Sodium levels matter. Low salt intake (like on a low-sodium diet) can cause lithium to accumulate. Don’t cut salt without talking to your doctor.
- Weight and hydration: Losing weight or becoming dehydrated (from illness, heat, or exercise) can spike lithium levels. Drink water consistently, especially in summer.
What Happens When You Switch Generics?
Pharmacists can legally swap your brand-name lithium for a generic without telling you. But if you’ve been stable for years, that switch could throw you off. In one case, four patients in a UK study had lithium levels spike to 1.32-1.88 mmol/L after their pharmacy switched their prescription to a different generic. All four developed symptoms: tremors, nausea, and dizziness. One needed hospitalization. Never assume a generic is interchangeable. If your pharmacy changes your pill, even if it’s still called “lithium carbonate,” ask your doctor to check your serum level within 1-2 weeks.
Why Some Doctors Still Prefer Brand-Name Lithium
Yes, generics cost less. But brand-name versions like Priadel and Camcolit come with detailed pharmacokinetic data. Their release profiles are consistent across batches. Generic manufacturers don’t always publish that information. A 2023 FDA draft guidance now requires manufacturers of extended-release lithium to prove equivalence through real-world blood tests-not just lab simulations. That’s a step forward. But until every generic is held to that standard, sticking with one brand (or one generic) is the safest bet.What’s Changing in 2025?
New research is making lithium therapy smarter. The International Consortium on Lithium Genetics (ConLiGen) has identified over 30 genes linked to how people respond to lithium. Some people naturally clear lithium faster. Others hold onto it longer. Several hospitals in the UK and US are now testing AI tools that use your age, weight, kidney function, and genetic markers to predict your ideal dose. In trials, these tools reduced the number of blood draws needed by 40% while keeping levels more stable. But until those tools are widely available, the old rules still apply: know your level. Know your pill. Know your body.What to Do If You’re on Lithium
Here’s your simple action plan:- Know which brand or generic you’re on. Write it down. Don’t let your pharmacy switch it without telling you.
- Get your serum lithium level checked every 3-6 months-more often if you’re adjusting doses or feeling off.
- Always test at the same time of day, 12 or 24 hours after your last dose.
- Keep a log: date, dose, level, symptoms (tremors, thirst, fatigue).
- Report any new meds, weight changes, or illness to your doctor immediately.
- Never stop lithium cold turkey. Tapering must be done slowly under supervision.
Lithium isn’t perfect. But for many people with bipolar disorder, it’s the most reliable tool they have. The key isn’t avoiding it-it’s mastering it. And that means paying attention to the numbers, not just the pills.
Can I switch between different lithium carbonate generics without checking my blood level?
No. Even if two generics have the same milligram dose, they can release lithium at different rates. Switching brands without checking your serum level can lead to toxicity or loss of effectiveness. Always ask your doctor to test your lithium level 1-2 weeks after any switch.
Why do I need to check my lithium level so often if I feel fine?
Lithium levels can rise slowly over time due to aging, reduced kidney function, or changes in diet and hydration. You might not feel symptoms until your level is dangerously high. Regular checks catch changes before you have a crisis.
Is lithium still used today, or are newer drugs better?
Lithium remains a first-line treatment for bipolar I disorder, especially for preventing suicide and long-term relapse. While newer drugs exist, none have matched lithium’s proven track record for preventing manic and depressive episodes over decades. About 60% of long-term bipolar patients still take it.
Can I take ibuprofen or other painkillers while on lithium?
Avoid NSAIDs like ibuprofen, naproxen, or diclofenac unless approved by your doctor. These drugs reduce kidney clearance of lithium, causing levels to rise quickly. Acetaminophen (paracetamol) is safer for pain relief.
What are the early signs of lithium toxicity?
Early signs include fine hand tremors, increased thirst, frequent urination, nausea, mild confusion, or muscle weakness. If you notice these, stop taking lithium and contact your doctor immediately. Severe symptoms like seizures, irregular heartbeat, or loss of consciousness require emergency care.
Do I need to avoid salt or fluids while on lithium?
No-don’t restrict salt or fluids. In fact, sudden drops in sodium intake (like on a crash diet) can cause lithium to build up in your blood. Eat normally and drink water consistently. Avoid dehydration, especially in hot weather or during illness.
Can lithium cause weight gain or thyroid problems?
Yes. Up to 50% of users gain weight over time, and 5-15% develop hypothyroidism. Regular thyroid tests (TSH every 6 months) can catch this early. If your thyroid slows down, you may need a simple hormone replacement-this doesn’t mean you have to stop lithium.
Is lithium safe for older adults?
Yes, but with caution. Older adults clear lithium more slowly and are more sensitive to side effects. Many doctors aim for lower targets-0.4-0.6 mmol/L-for patients over 60. More frequent monitoring is essential.
If you’re on lithium, you’re not alone. Thousands of people manage bipolar disorder with it every day. The key isn’t fear-it’s awareness. Know your numbers. Know your pill. And never stop checking.
9 Comments
Write a comment
More Articles
Hydroxyurea, Bone Health & Osteoporosis: Prevention & Management Guide
Learn how hydroxyurea can affect bone health, recognize osteoporosis risks, and follow practical steps-diet, exercise, screening, and meds-to keep your bones strong while on therapy.

Tadacip (Tadalafil) vs Other ED Pills: Complete Comparison Guide
A thorough comparison of Tadacip (tadalafil) with sildenafil, vardenafil, avanafil, and generic tadalafil, covering onset, duration, side effects, cost and how to choose the best ED pill.
The Role of Antiviral Medications in Shingles Treatment
As a blogger, I've recently come across an interesting topic - the role of antiviral medications in shingles treatment. Shingles is a painful skin rash caused by the varicella-zoster virus, the same virus responsible for chickenpox. Antiviral medications play a crucial role in treating shingles by reducing the severity and duration of the symptoms. They work best when taken early in the course of the illness, ideally within 72 hours of the rash appearing. In conclusion, antiviral medications are an essential component in shingles treatment, providing relief and preventing complications.
Himanshu Singh
December 29, 2025 AT 20:09man i just switched generics last month and thought i was fine til i started getting shaky hands and drinking like a camel 😅 turns out my level jumped to 1.3-thank god i checked. never assume the pill looks the same means it works the same. write it down, folks.