
When your hip starts to ache with every step, it’s not just about aging. It’s often osteoarthritis - and excess weight is one of the biggest drivers behind it. Unlike knee osteoarthritis, where weight loss clearly helps, the connection between losing weight and hip pain relief has been messy, confusing, and even contradictory. But new research is changing the story. If you’re carrying extra pounds and struggling with hip pain, this isn’t just about looking better - it’s about saving your joint before it’s too late.
Why Your Hip Hurts When You’re Overweight
Osteoarthritis of the hip isn’t just "wear and tear." It’s a full breakdown of the cartilage that cushions the ball-and-socket joint. Bone starts to rub on bone. Inflammation creeps in. The joint swells, stiffens, and loses function. And while aging plays a role, obesity is the silent accelerant. For every extra pound you carry, your hip joint takes on 3 to 4 times that load during walking. That’s not just pressure - it’s constant trauma.
Studies show that people with a BMI over 30 are far more likely to develop hip osteoarthritis. In fact, if obese men dropped into the overweight range and overweight men reached normal weight, hip OA rates could fall by over 30%. The numbers are even higher for women. This isn’t theoretical. It’s biomechanical. Your hip joint doesn’t just support your weight - it absorbs shock, rotates, and moves under load. Extra fat doesn’t just add mass; it changes how your whole body moves, straining muscles, tendons, and ligaments around the joint.
Weight Loss Isn’t Just for Knees - It Works for Hips Too
For years, doctors told people with hip OA: "Lose weight if you can, but don’t expect much change." That belief came from a few small studies that showed little to no improvement in hip pain after weight loss. One 2023 trial compared a very-low-calorie diet with exercise against exercise alone. At six months, there was no meaningful difference in hip pain between the groups. That study got a lot of attention - and even led a major medical journal to declare, "Osteoarthritis of the Hips Is Unaffected by Weight Loss." But here’s what they missed: time.
A follow-up at 12 months changed everything. The group that lost weight didn’t just feel better - they had significantly less pain, better mobility, and higher scores on quality-of-life measures. The benefits didn’t show up fast. They built up. And they were real.
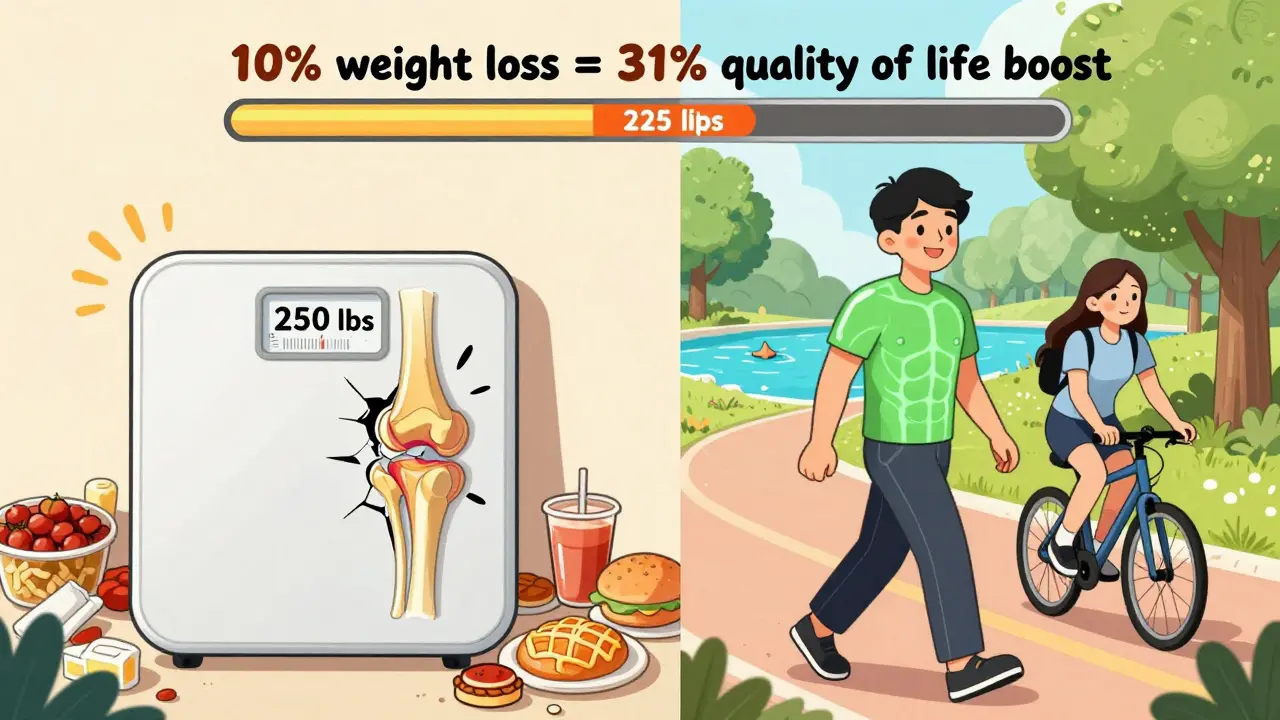
Then came the 2024 Nature study - the most detailed look yet. Researchers tracked 65-year-olds with hip OA and obesity. Those who lost more than 10% of their body weight saw dramatic improvements across every measure: pain, stiffness, daily function, and even quality of life. The biggest jump? A 31% improvement in how they felt about their hip-related quality of life. That’s not a fluke. That’s a transformation.
And here’s the kicker: losing 5% helped. Losing 7% helped more. But losing over 10%? That’s where the real shift happened. It wasn’t just less pain. It was the ability to walk without fear, climb stairs without hesitation, and sleep through the night.
How Much Weight Do You Actually Need to Lose?
For knee osteoarthritis, experts say losing 5% of your body weight can cut pain in half. For hips? That number doesn’t hold up. The data says: aim for 10% or more.
Here’s what that looks like:
- If you weigh 200 pounds, losing 20 pounds could mean the difference between limping and walking normally.
- If you weigh 250, losing 25 pounds might get you off painkillers and back into your favorite activities.
And here’s the surprising part: losing 20% didn’t give you much more benefit than losing 10%. That means there’s a sweet spot. You don’t need to become skinny. You just need to get out of the obese range. The goal isn’t perfection - it’s function.
One study tracked 35 people with hip OA and a BMI over 25. After eight months of combined exercise and diet, they lost an average of 10% of their body weight - and saw a 32.6% improvement in physical function. That’s not magic. That’s science.
Exercise Isn’t Optional - It’s Essential
Weight loss alone isn’t enough. If you drop weight but don’t move, your muscles weaken, your joint still deteriorates, and pain comes back. You need both.
The best approach? Low-impact movement that builds strength without pounding your hip:
- Swimming or water aerobics - zero impact, full range of motion
- Cycling (stationary or outdoor) - smooth, controlled, joint-friendly
- Strength training for glutes and thighs - stabilizes the hip joint
- Walking - start short, build up slowly
Avoid high-impact activities like running, jumping, or heavy squats. They don’t help - they hurt. And don’t wait until you’ve lost weight to start moving. Begin now. Even 20 minutes a day of gentle activity can reduce inflammation, improve circulation, and protect your cartilage.
What About Diet? What Really Works
Not all diets are created equal. A low-carb approach, backed by the Journal of Metabolic Health, showed the best results for hip OA patients. Why? Because it reduces inflammation, stabilizes blood sugar, and helps control hunger without extreme hunger.
Here’s what to focus on:
- More vegetables, especially leafy greens and cruciferous ones like broccoli and cauliflower
- Healthy fats - olive oil, avocado, nuts, fatty fish like salmon
- Lean protein - chicken, tofu, eggs, legumes
- Whole grains - oats, quinoa, brown rice
- Less sugar, less processed food, less refined carbs
Forget calorie counting. Focus on food quality. A 2024 study showed that people who ate real, whole foods lost more weight - and kept it off - than those on rigid calorie-restricted diets. Your body doesn’t respond to numbers. It responds to nutrients.
What If You Can’t Lose Weight?
Some people try everything - diet, exercise, support groups - and still struggle. That doesn’t mean you’re out of options.
Medications like semaglutide (Wegovy) and tirzepatide (Zepbound) are now FDA-approved for weight loss in people with a BMI over 30 - or over 27 with other risk factors like hip OA. These drugs aren’t magic pills. They work best when paired with lifestyle changes. But for those who’ve tried everything else, they can be a lifeline.
And here’s the truth: even if you can’t lose 10%, losing 5% still helps. Every pound matters. Progress isn’t all-or-nothing.
Joint Preservation: The Real Goal
The goal isn’t just to feel better today. It’s to avoid surgery tomorrow. Hip replacements are common - but they’re not permanent. They wear out. They can fail. They require recovery. And once you have one, your body changes forever.
Weight loss and exercise don’t just reduce pain. They slow down the destruction of cartilage. They take pressure off the joint. They strengthen the muscles that support it. They delay the need for surgery - sometimes by decades.
Think of it like this: your hip is a car. Excess weight is like driving with a flat tire. You can keep going, but you’re wearing out the rim. Weight loss? That’s fixing the tire. Exercise? That’s getting an alignment. Together, they let your joint last longer.
What’s Next? Start Here
You don’t need a gym membership. You don’t need a personal trainer. You just need to start.
Here’s your simple 3-step plan:
- Track your weight and symptoms - Write down your weight every week and rate your hip pain on a scale of 1 to 10.
- Move daily - Walk 20 minutes, swim 15 minutes, or ride a bike. Do it even if it hurts a little. Movement is medicine.
- Eat real food - Swap one processed snack for an apple. Replace soda with water. Add one extra vegetable to your plate.
Do this for 3 months. Then check in. You’ll be surprised how much better you feel.
There’s no cure for hip osteoarthritis. But there is a way to stop it from getting worse. And it starts with what you eat, how much you move, and how much weight you carry.
It’s not about being thin. It’s about being strong. Mobile. Independent. And free from pain.
Can weight loss reverse hip osteoarthritis?
No, weight loss won’t reverse cartilage damage that’s already happened. But it can stop it from getting worse. It reduces inflammation, takes pressure off the joint, and improves mobility - which means you may not need surgery for years, or ever.
Is walking good for hip osteoarthritis?
Yes - if done correctly. Walking is low-impact and helps keep the joint moving. Start with short walks (10-15 minutes), use supportive shoes, and avoid uneven surfaces. If it hurts badly, stop and try swimming or cycling instead.
How long does it take to see results from weight loss for hip pain?
Some people feel better in 4-6 weeks, especially in stiffness and morning pain. But major improvements in function and pain usually take 3-6 months. The 2024 Nature study showed the biggest gains happened after 12 months. Patience matters.
Should I try a very-low-calorie diet for hip OA?
Only under medical supervision. Very-low-calorie diets can lead to quick weight loss, but they’re hard to maintain and may cause muscle loss if not paired with strength training. The 2023 trial showed better results after 12 months, not 6. Long-term habits beat short-term extremes.
Do I need to lose weight if I’m only slightly overweight?
Even a 5% loss helps - but 10% makes a bigger difference. If your BMI is over 25 and you have hip pain, losing even 10-15 pounds could reduce your pain significantly. You don’t need to be at your ideal weight - just lighter than you are now.
Final Thought: It’s Not Too Late
Many people with hip osteoarthritis think surgery is their only option. They wait until the pain is unbearable. But the truth is, your joint is still salvageable - if you act now. You don’t need to be perfect. You just need to be consistent. Eat better. Move more. Lose weight. Protect your hip. And keep walking - not just for today, but for years to come.
15 Comments
Write a comment
More Articles
Topiramate Withdrawal: Symptoms and Tips for Managing Them
In my latest article, I discuss the process of withdrawing from Topiramate, a medication typically used for treating epilepsy and migraines. The withdrawal can lead to various symptoms including anxiety, restlessness, and sleep disturbances. I also provide useful tips to manage these symptoms, such as tapering off the dosage gradually under a doctor's guidance and maintaining a healthy lifestyle. It's important to remember that everyone's experience is different, so don't hesitate to seek professional help if needed. Understandably, this process can be challenging, but with the right approach and support, it can become manageable.


John Watts
February 10, 2026 AT 00:35Man, this post hit different. I lost 28 pounds over a year after my hip started screaming every morning, and let me tell you - it wasn’t just about pain. It was about standing up from a chair without grunting. I started with walking 15 minutes a day, no matter how bad it hurt. Now? I hike with my kids. No surgery. No fancy meds. Just consistency. You don’t need to be perfect - just show up.
And yeah, 10% is the magic number. I hit 10.5%. That’s all it took. Not 20. Not 30. Just enough to stop feeling like a loaded freight train with legs.