Folate deficiency: what it looks like and how to fix it
Feeling tired, pale, or short of breath and not sure why? Low folate (vitamin B9) is a common, treatable cause. This guide shows what usually causes folate deficiency, the signs to watch for, how doctors test for it, and simple, practical fixes you can start today.
Causes and who’s at risk
Folate can drop because you don’t eat enough folate-rich foods, your body can’t absorb it, or your needs are higher. Pregnancy raises folate needs a lot. Alcohol abuse, poor diet, and malabsorption conditions like celiac disease also lower folate. Certain medicines — for example, methotrexate, some anti-seizure drugs, and trimethoprim — interfere with folate. Older adults and people who’ve had weight-loss surgery can be at greater risk too.
Note: folate in food is different from folic acid, the stable form in supplements and fortified foods. Both help, but they behave slightly differently in the body.
Symptoms, tests, and red flags
The most common sign is megaloblastic anemia — that means tiredness, weakness, breathlessness, and pale skin. Blood tests often show a high mean corpuscular volume (MCV), usually over about 100 fL, and low serum or red blood cell (RBC) folate. RBC folate gives a better picture of body stores than serum folate.
Some people notice mouth sores, a swollen tongue, or trouble concentrating. Before starting high-dose folic acid, doctors usually check vitamin B12 because folic acid can correct the anemia but won’t stop B12-related nerve damage. If you have tingling, numbness, balance problems, or other nerve symptoms, get B12 checked right away.
Severe symptoms like fainting, very fast heartbeat, chest pain, or sudden confusion need urgent care. Mild cases can be handled with outpatient treatment and follow-up.
Treatment is straightforward: replace the folate and fix the cause. For prevention, most adults are advised about 400 mcg (0.4 mg) folic acid daily. Pregnant people should take about 600 mcg daily to reduce neural tube defect risk. For confirmed deficiency, doctors commonly prescribe 1 mg (1000 mcg) of folic acid daily for a few months; sometimes higher doses are used under supervision. Always follow a clinician’s plan.
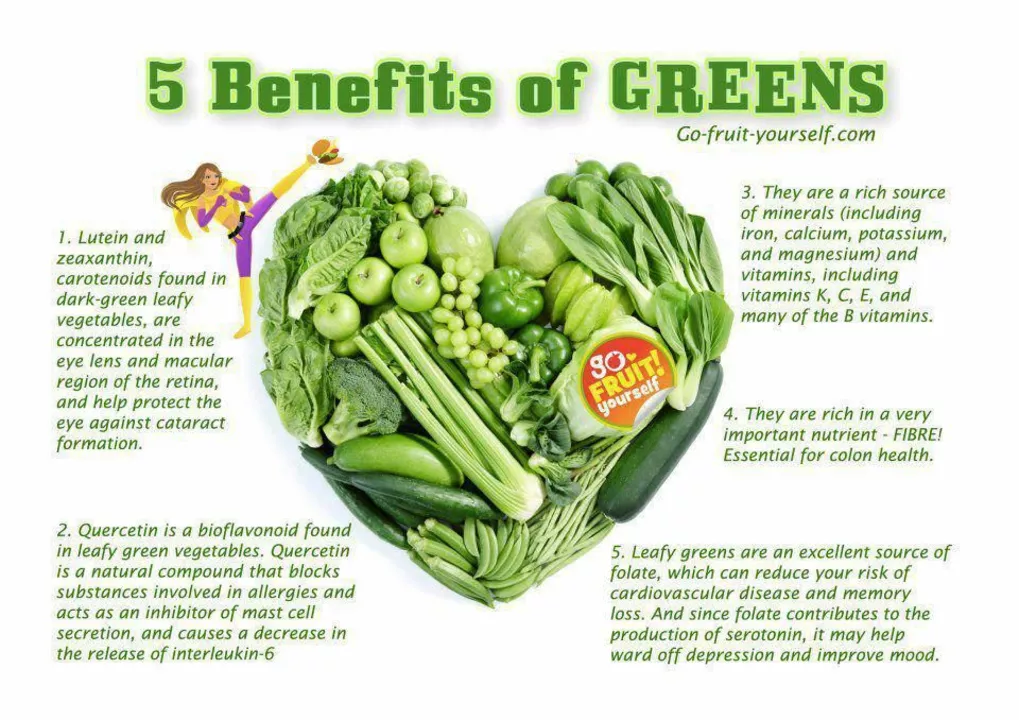
Food helps too. Eat leafy greens (spinach, kale), beans and lentils, asparagus, broccoli, and fortified cereals. If medication or absorption issues are the reason, dietary change alone may not fix it — you’ll likely need supplements and medical follow-up.
Want to avoid a repeat? If you’re on medications that affect folate, pregnant or planning pregnancy, drink heavily, or have digestive conditions, mention folate screening to your doctor. A simple blood test and a short supplement course often keep you out of trouble and feeling better fast.
If you’re unsure whether your symptoms come from folate or something else, get checked. These problems are common and treatable — and catching them early makes a big difference.
Folate Deficiency and Eye Health: What You Need to Know
As a blogger, I recently came across an important topic concerning eye health - folate deficiency. Folate, also known as vitamin B9, plays a crucial role in maintaining our overall well-being, including our precious eyesight. A deficiency in folate can lead to various eye problems, such as macular degeneration and optic neuropathy. To prevent these issues, it's essential to consume a balanced diet rich in leafy greens, beans, and fortified cereals. So, let's take care of our eyes by ensuring we get enough folate in our daily diets!