Parkinson's disease: practical guide for patients and caregivers
Parkinson's disease is a brain disorder that changes movement, mood, and sleep. If you or someone close has been diagnosed, you probably want clear, useful steps — not medical jargon. Here are straightforward tips on symptoms to watch for, treatments that actually help, and daily habits that make life easier.
Early signs often include a slight tremor in one hand, stiffness, slower movements, or balance changes. Non-motor signs can be low mood, sleep trouble, constipation, or a softer voice. Not every case looks the same. Keep a simple symptom diary: note when symptoms start, what makes them worse, and how long they last. That helps your doctor adjust treatments faster.
Common treatments and what to expect
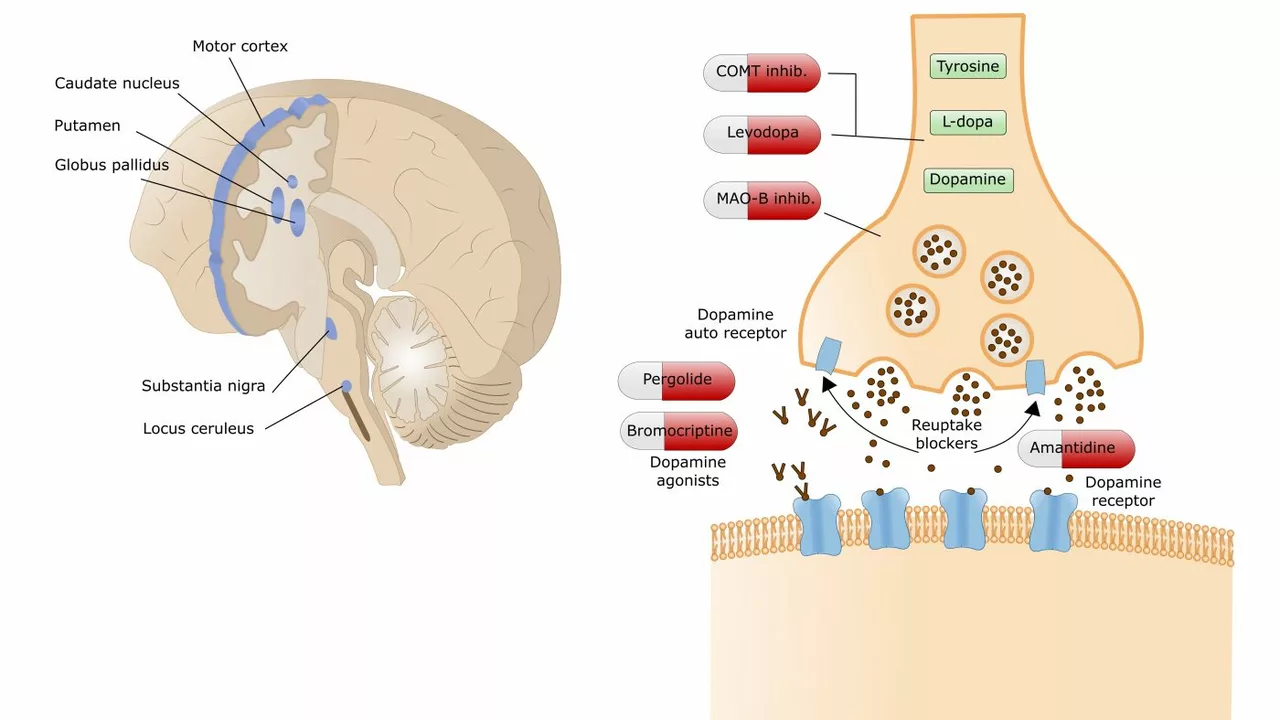
Levodopa is still the most effective drug to reduce slowness and stiffness. Doctors may add dopamine agonists, MAO-B inhibitors, or amantadine depending on symptoms and side effects. Amantadine can help with movement and some medicines for restless legs; it shows up in new RLS research and is useful for some Parkinson's patients too. If drugs stop working well, options include changing timing, using controlled-release forms, or discussing advanced therapies like deep brain stimulation with a specialist.
Medication timing matters. Many people feel better when doses match daily routines — take notes on "good" and "off" periods. Also watch for interactions: some antidepressants and herbal supplements affect Parkinson's medicines. Always tell clinicians about every medicine, including over-the-counter drugs.
Daily life: practical tips
Exercise helps more than you expect. Balance work, walking, tai chi, or simple strength exercises into your week — aim for short daily sessions. Physical and speech therapy can improve walking, reduce falls, and keep your voice clearer. Small home changes cut risk: remove loose rugs, add grab bars, use non-slip mats, and keep rooms well lit.
Mood and thinking changes are real parts of Parkinson's for many people. Talk openly with your care team about anxiety, depression, or memory shifts. Social support matters: join a local support group or an online forum where members share tips on routines and coping tricks. Caregivers should plan short breaks and accept help — burnout hurts both of you.
When to see a specialist: if symptoms progress, medications cause confusing side effects, or daily activities become hard, ask for a neurology or movement-disorder clinic referral. Bring your symptom diary and a current medication list. Quick adjustments often make big differences.
If you want reliable follow-up reading, check articles on restless legs updates, amantadine use, and therapies that improve sleep and movement. Small, steady steps — smarter meds, daily exercise, and reasonable home changes — often deliver the biggest gains in comfort and independence.
Practical checklist: 1) Keep a medication schedule and pill box. 2) Track mobility and mood each week. 3) Schedule yearly vision and hearing checks. 4) Talk about fall prevention with your therapist. 5) Ask about clinical trials if treatments stop working. Small planning saves time and reduces stress for you and your family.
Keep questions ready for every visit and notes.
The potential benefits of betahistine for individuals with Parkinson's disease
In my recent exploration, I discovered the potential benefits of Betahistine for those living with Parkinson's disease. This medication, often used for vertigo, could potentially improve symptoms of this neurodegenerative condition. Researchers suggest that Betahistine might have the ability to reduce tremors and improve motor function. There is also a belief that it could enhance cognitive abilities and alleviate depression often associated with Parkinson's disease. However, it's important to note that more research is needed to confirm these potential benefits.