Medication Side Effect Risk Calculator
Enter your situation to see your side effect risk score. The calculator uses real-world data from the article to show how telehealth interventions reduce risk.
Your Risk Score
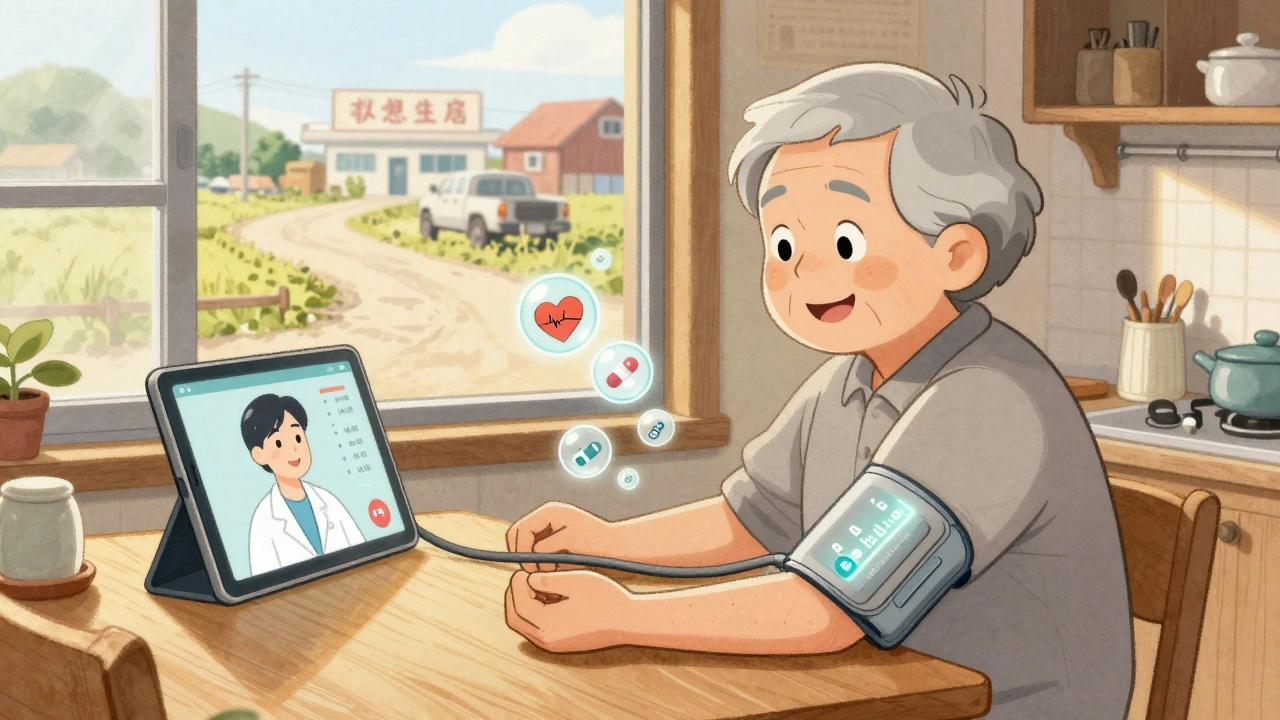
For millions of people living in rural and remote areas, taking medication for chronic conditions like high blood pressure, depression, or blood clots comes with a hidden risk: side effects. These reactions can be dangerous, even life-threatening. But getting to a doctor for a check-up? That might mean driving 70 miles over dirt roads, taking half a day off work, or waiting weeks for an appointment. In many cases, patients don’t report symptoms until it’s too late. That’s where telehealth comes in-not as a luxury, but as a lifeline.
Why Rural Patients Are at Higher Risk
Rural patients face a perfect storm when it comes to medication safety. According to the Health Affairs analysis from 2020, they experience 23% more preventable adverse drug events than people in cities. Why? It’s not just distance. Many rural clinics are understaffed. Pharmacists are scarce. Emergency care is hours away. And nearly 42% of people in frontier areas don’t have reliable broadband, making even simple video calls impossible. Worse, 36% of rural adults have low health literacy. They might not know what ‘dizziness’ or ‘bruising easily’ means in relation to their blood thinner. They might think fatigue is just aging. Or they might be too proud to admit they’re struggling. In urban settings, patients can walk into a pharmacy or clinic. In rural areas, silence often means danger.How Telehealth Monitoring Actually Works
Modern telehealth for side effect monitoring isn’t just a Zoom call. It’s a system. A network of tools working together to catch problems before they become emergencies. At the core are remote patient monitoring (RPM) devices. These include Bluetooth-enabled blood pressure cuffs, smart scales that track fluid weight, and wearable heart rate monitors. Devices like those from Yosi Health are FDA-cleared and accurate within ±3% for blood pressure and ±2 beats per minute for heart rate. Patients use them daily at home. Data syncs automatically to a secure platform. Then there’s the human side. Weekly video visits with a pharmacist or nurse. Patients report symptoms like nausea, tremors, or confusion. If a patient’s INR (a blood clotting measure) spikes on their monitor, the system alerts the care team immediately. In one program at the University of Mississippi, this caught dangerous bleeding risks before symptoms appeared-saving lives. Medication adherence is tracked too. Smart pill dispensers like Hero Health open only at scheduled times and log when doses are taken. If a patient misses a dose, the system sends a text reminder. If they miss two in a row, a nurse calls. Studies show this boosts adherence from 62% to 89%.What Works Best: Real-World Examples
Not all telehealth programs succeed. The difference? Structure. The University of Mississippi’s anticoagulation program uses three key pieces: a Bluetooth INR monitor, weekly pharmacist video visits, and a care coordinator who follows up with patients who miss appointments. Result? 92% of patients stay in the program for over a year. In Arkansas, a pilot program uses wearable sensors to detect subtle movement changes in patients taking antipsychotic drugs. These sensors pick up early signs of tardive dyskinesia-a side effect that can become permanent if not caught. The system detected issues with 91% accuracy in early tests. Even audio-only calls are making a difference. Since the 2023 CONNECT for Health Act, Medicare now covers phone check-ins for side effect monitoring. That’s huge for seniors who don’t have smartphones or reliable internet. In rural West Virginia, one program saw a 30% increase in follow-up rates just by switching to phone calls.
The Tech That Makes It Possible
You don’t need fancy gear. Most patients use smartphones they already own. The apps work on iOS 14+ and Android 10+, which cover 92% of phones in use today. But here’s the catch: 28% of rural Americans still lack broadband that meets FCC standards. And 34% of seniors say they struggle to use the apps. That’s why successful programs don’t just hand out an app and walk away. They train patients. The average patient needs two to four sessions to feel confident. Older adults need an average of 3.2 sessions. Nurses spend 47 minutes per person during setup-teaching how to use the device, how to interpret the data, and when to call for help. Security matters too. All video platforms use end-to-end AES-256 encryption. Data is stored on HIPAA-compliant servers. No one’s listening in. No one’s selling your info.What’s Missing: The Gaps in the System
Telehealth isn’t magic. It can’t replace everything. About 22% of side effects require physical touch-like checking for swelling in the legs, feeling for lymph nodes, or listening to heart sounds. These still need in-person visits. That’s why the best programs combine remote monitoring with scheduled local check-ups. Communication gaps are another problem. A patient in West Virginia once complained their video call was too blurry to see their tremors. The provider missed a key sign of a drug reaction. That’s why some clinics now use photo uploads-patients snap a picture of a rash or swelling and send it ahead of time. And then there’s the economic side. Urban telehealth companies are expanding into rural markets. They offer cheaper, faster care. But that’s hurting local clinics. A 2022 study found that when urban providers enter a rural area, local hospital revenue drops by 15%. That means fewer staff, fewer services, and less sustainability for the very programs rural patients depend on.Who’s Leading the Way
Pharmacists are becoming the backbone of rural telehealth. The American Pharmacists Association says pharmacist-led monitoring programs achieve 89% adherence. That’s 27 points higher than standard care. At Vanderbilt University, adding pharmacists to telehealth teams cut severe side effects by 43%. The FDA just approved AI tools like IBM Watson’s MedSafety system. It scans patient-reported symptoms and lab data to predict which patients are at risk of a bad reaction-84% accuracy, according to a 2023 NEJM study. It doesn’t replace the doctor. It flags the red flags before they turn into emergencies. Pharmaceutical companies are stepping in too. Pfizer and Merck have spent $450 million since 2022 on telehealth programs for rural patients. Why? Because better adherence means fewer hospitalizations-and that’s good for patients and for their bottom line.
What Patients Say
Real people have real stories. One patient in Montana, on a blood thinner, said: “The app caught my INR climbing before I felt sick. I got a call within an hour. They adjusted my dose. I didn’t end up in the ER.” Another, from rural Alabama, said: “I used to drive 90 miles every month for my antidepressant check-up. Now I do it from my kitchen table. I’ve missed only one appointment in two years.” But not all feedback is positive. Some say it feels impersonal. Others can’t get the app to work. One woman in Ohio said: “I’m 72. I don’t know what ‘sync’ means. I gave up.” The common thread? Convenience and reduced travel are the biggest wins. Patients save an average of 72 miles per visit. That’s hours saved. Gas money saved. Stress saved.How to Make It Work in Your Community
If you’re a clinician, a caregiver, or even a patient trying to get better care:- Start with the most dangerous medications: anticoagulants, antihypertensives, and psychotropics. These account for 68% of high-risk drug use in rural areas.
- Use simple tools first: Bluetooth devices that auto-send data. No complex apps.
- Train patients in person, if possible. One-on-one help cuts failure rates in half.
- Use audio-only calls for seniors who can’t use video.
- Partner with local pharmacists. They’re the most accessible health professionals in many towns.
- Build tiered responses: call immediately for chest pain, within 24 hours for nausea, within 72 hours for mild headaches.
- Push for local reimbursement. CMS pays $51 for 20 minutes of remote monitoring. But only 63% of private insurers follow that rate. Advocate for change.
The Future Is Here-But It’s Not Equal Yet
Telehealth for side effect monitoring isn’t the future. It’s happening now. In 2023, 47% of rural clinics use it. By 2025, 92% plan to expand. But progress isn’t automatic. Black rural patients are 1.8 times less likely to get these services than white patients. Broadband gaps still leave entire counties offline. Staffing shortages mean nurses are stretched too thin. The solution isn’t just better tech. It’s better policy. Fairer pay. Local investment. Community trust. For rural patients, telehealth isn’t about convenience. It’s about survival. The right system can catch a dangerous side effect before it’s too late. It can keep someone out of the hospital. It can let them stay in their home, in their community, with dignity. It’s not perfect. But it’s better than nothing. And with the right support, it can be everything.12 Comments
Write a comment
More Articles

Buy Cheap Generic Zyrtec Online - Safe Guide & Best Prices 2025
Learn how to safely buy cheap generic Zyrtec online in the UK. Get a step‑by‑step guide, price comparison, safety tips, and a checklist to avoid scams.

Unleash the Potential of Rose Hip Supplements for a Healthier You
I recently discovered the incredible potential of rose hip supplements for boosting our overall health. These natural supplements are packed with essential nutrients like vitamin C, antioxidants, and anti-inflammatory properties. By incorporating rose hip supplements into our daily routine, we can strengthen our immune system, improve skin health, and reduce inflammation in our bodies. I'm genuinely excited to share my findings with you all, and I encourage you to explore the benefits of rose hip supplements for a healthier you. Let's embrace this natural remedy and unlock our true potential!

Iris Carmen
December 10, 2025 AT 08:41i just got my bp cuff from yosi last month and honestly it’s been a game changer. no more driving 45 mins just to check if my meds are working. i even showed my mom how to use it and she’s 71 and she figured it out in like 10 mins.
also the text reminders? genius. i forgot my pill twice last week and got a text before i even realized. no shame.