Many people are told to switch from a brand-name medicine to a generic version-and they panic. Generic medications look different. They cost a lot less. And suddenly, you’re wondering: Is this really the same? Will it work? Could it hurt me?
The short answer? Yes, it’s the same. And no, it won’t hurt you-if you’re taking it as prescribed. But the fear is real. And it’s not just in your head. It comes from stories, old habits, and misinformation that’s been passed down like family recipes. Let’s clear up the biggest concerns, one by one.
Are generic drugs really as effective as brand-name ones?
Yes. Absolutely. The U.S. Food and Drug Administration (FDA) doesn’t approve a generic drug unless it delivers the exact same amount of active ingredient into your bloodstream at the same rate as the brand-name version. That’s called bioequivalence. The FDA requires testing to prove that the generic’s absorption falls within 80% to 125% of the brand-name drug’s levels. That’s not a guess. It’s science. And it’s strict.
Think of it like this: two different brands of aspirin both contain acetylsalicylic acid. One might be shaped like a capsule, the other a flat tablet. One might be white, the other blue. But they both dissolve the same way and do the same job. That’s what generics are.
Over 90% of all prescriptions in the U.S. are filled with generics. That’s not because pharmacies are cutting corners. It’s because they work. Studies show that for the vast majority of conditions-high blood pressure, diabetes, cholesterol, depression-generics perform just as well as the name-brand versions.
Why do generics look different?
Because the law says they have to. Brand-name drugs have trademarks-not just on the name, but on the shape, color, and even the imprint on the pill. Generic manufacturers can’t copy that. So they make theirs look different. That’s it. No hidden reason. No trick.
That difference in appearance is why some patients think they got the wrong medicine. A woman I spoke with in Birmingham told me she switched from her blue Eliquis pill to a white one and refused to take it for a week. She thought the pharmacy made a mistake. When she checked, the generic was approved by the FDA, had the same active ingredient, and cost 85% less. She started taking it. Her blood thinner worked just fine.
Don’t let the color or shape fool you. Check the label. Look for the active ingredient. If it matches, you’re good.
Do generics have more side effects?
No. But here’s where confusion creeps in.
Generics use the same active ingredient as the brand-name drug. That’s the part that treats your condition. But they can use different fillers, dyes, or coatings-called excipients. These don’t affect how the drug works. But if you’re allergic to a specific dye or lactose, you might react to one version and not the other.
That’s rare. And it’s not because generics are lower quality. It’s because the ingredients in the pill’s outer shell vary. If you’ve had a reaction to a new generic, talk to your pharmacist. They can check if the excipients changed and suggest another generic version that matches your tolerance.
Also, side effects aren’t new when you switch. They’re just noticed more. When you’ve been on a brand-name drug for years, your body adjusts. Switching-even to an identical drug-can make you hyper-aware of how you feel. That’s psychology, not pharmacology.

Can generics be counterfeit or contain less active ingredient?
No. Not if they’re sold legally in the U.S., UK, or other regulated markets. The FDA requires every generic manufacturer to prove their product contains the exact same active ingredient, in the exact same strength, as the brand-name drug. They must also prove it’s manufactured under the same strict quality controls.
There’s a myth that generics are made in cheaper factories with lower standards. That’s not true. In fact, about half of all generic drugs are made by the same companies that make the brand-name versions. Pfizer, Merck, and Johnson & Johnson all produce generics. The only difference? They’re not paying for advertising or fancy packaging.
The FDA inspects generic drug factories just as often as brand-name ones. Since 2018, their Risk Identification and Correction Action Program has fixed over 1,200 potential quality issues-most of them in generic plants. That’s oversight, not neglect.
Why are generics so much cheaper?
Because they don’t have to pay for research, development, or marketing.
Brand-name companies spend billions creating a new drug. They run clinical trials, hire scientists, patent the formula, and run TV ads. That cost gets built into the price.
Generic companies? They just copy the formula after the patent expires. They don’t need to repeat expensive trials. They only need to prove bioequivalence-which costs a fraction. And once one generic enters the market, others follow. More competition = lower prices.
The result? Generics cost 80% to 85% less on average. Over the past decade, they’ve saved the U.S. healthcare system over $2.2 trillion. That’s not just money for insurance companies. It’s money in your pocket. Lower copays. Fewer skipped doses because you can’t afford it.
Are there exceptions? When should I stick with brand-name?
Yes. A small group of drugs requires extra care. These are called narrow therapeutic index (NTI) drugs. That means the difference between a dose that works and a dose that’s dangerous is very small.
Examples include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin and levetiracetam (anti-seizure meds)
For these, some doctors prefer to keep you on the same version-brand or generic-once you’re stable. Why? Because even tiny differences in absorption could, in rare cases, affect how well the drug controls your condition.
But here’s the key: switching from brand to generic, or between generics, is still safe-if monitored. Your doctor or pharmacist should check your blood levels or symptoms after the switch. A 30-day follow-up is standard practice for NTI drugs. Don’t assume you’re on your own. Ask for a check-in.
And remember: if your doctor writes “Do not substitute” on your prescription, the pharmacy must honor it. That’s the law.
Why do some people distrust generics?
It’s not just about science. It’s about trust.
A 2014 survey found that while most people believed generics were safe and effective, 16% still doubted them. And among non-Caucasian patients, the doubt was much higher-56% asked for brand-name drugs, compared to 43% of others.
Why? Stories. Word of mouth. A friend said their generic made them dizzy. A relative swore their old brand was better. These aren’t lies. They’re experiences. But they’re not always about the drug. Sometimes, it’s stress, aging, diet changes, or other meds that caused the side effect-and it got blamed on the switch.
Pharmacists are often the first line of defense. When you pick up your prescription, ask: “Is this the same as my old one?” They can explain the difference in appearance. They can confirm the active ingredient. They can reassure you. Don’t just walk away. Ask.
What should I do if I think the generic isn’t working?
Don’t stop taking it. Don’t switch back without talking to someone.
First, give it time. Your body might need a few weeks to adjust. Even if the drug is identical, your perception of how you feel can change.
Second, track your symptoms. Write down how you feel before and after the switch. Are you having more headaches? More fatigue? More anxiety? Or are you just noticing things you didn’t before?
Third, call your pharmacist. They can check if the generic changed manufacturers. Sometimes, a different version is substituted without your knowledge. They can also tell you if your insurance switched the preferred generic.
Fourth, schedule a quick check-in with your doctor. They can order a blood test if needed-especially for NTI drugs. Most of the time, the generic is working fine. But if it’s not, you’ll know why-and what to do next.
Final thought: Your health matters. So does your wallet.
Choosing a generic isn’t settling. It’s smart. It’s safe. And it’s backed by decades of science and millions of patients.
Generic drugs have been used by over 90% of Americans who take prescription medicine. They’re not second-rate. They’re second-generation-built on the same science, with the same standards, and without the marketing markup.
If you’re unsure, ask. Ask your pharmacist. Ask your doctor. Ask a friend who’s been on generics for years. Chances are, they’ll tell you they’ve never had a problem.
Medicine doesn’t have to be expensive to be effective. Sometimes, the best treatment is the one you can actually afford to take every day.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, strength, purity, and potency as brand-name drugs. They must prove bioequivalence, meaning they deliver the same amount of active ingredient into your bloodstream at the same rate. Generic drugs are tested and inspected just like brand-name drugs.
Why do generic pills look different from brand-name ones?
By law, generic manufacturers can’t copy the exact appearance of brand-name pills, including color, shape, or markings, because those are trademarked. But the active ingredient-and how it works in your body-is identical. The difference is only in the outer shell, which doesn’t affect effectiveness.
Can generic drugs cause more side effects?
Not because they’re generic. Side effects come from the active ingredient, which is the same. But generics may use different inactive ingredients (like dyes or fillers), which could cause rare allergic reactions in sensitive individuals. If you notice new side effects after switching, talk to your pharmacist-they can help identify the cause.
Are there any drugs where I shouldn’t switch to a generic?
For a small group of drugs called narrow therapeutic index (NTI) drugs-like warfarin, levothyroxine, and some anti-seizure medications-small changes in absorption can matter. Doctors may recommend staying on the same version (brand or generic) once you’re stable. Always discuss switching with your provider, and get follow-up tests if needed.
How do I know if my pharmacy switched my generic?
Check the label on your pill bottle. It will list the manufacturer and the generic name. If you notice a change in size, color, or shape, ask your pharmacist. They can confirm whether a different generic version was dispensed. You can also ask for the brand-name version if you prefer-but it may cost more.
Can I trust generics made overseas?
Yes. Many generic drugs, both brand and generic, are manufactured overseas-including in India and China. The FDA inspects all facilities, regardless of location, to ensure they meet U.S. quality standards. A drug’s origin doesn’t determine its safety. What matters is FDA approval and compliance.
Why do some doctors still prescribe brand-name drugs?
Sometimes, it’s habit. Other times, they’re unaware a generic is available. Or, for NTI drugs, they prefer to maintain consistency. In some cases, insurance doesn’t cover the generic yet. If you’re unsure, ask your doctor: “Is there a generic available? Would it be safe for me?”
14 Comments
Write a comment
More Articles
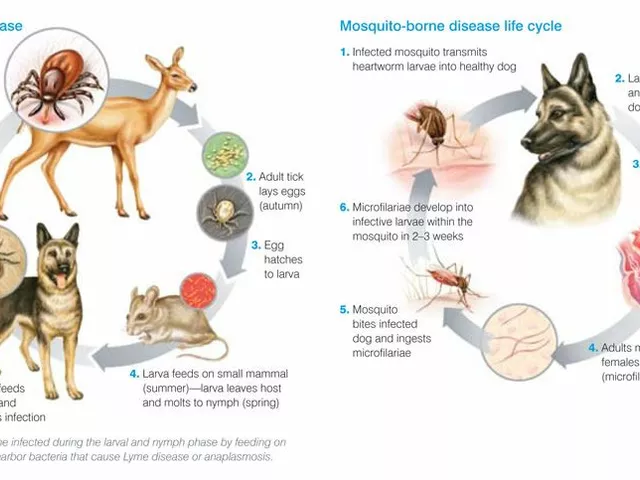
Tick Fever: What You Need to Know About This Dangerous Disease
Tick Fever, also known as Tick-Borne Disease, is a serious illness transmitted by ticks. It's crucial to be aware that this disease can have severe health implications including fever, headache, and fatigue, and in some cases can even be fatal. Early detection and treatment are absolutely vital. It's also important to take steps in preventing tick bites, such as using repellents and wearing appropriate clothing when in tick-infested areas. Stay safe out there, folks!

Sylvia Frenzel
December 11, 2025 AT 09:21I don't care what the FDA says. My cousin took a generic blood pressure pill and ended up in the ER. They don't test these things long enough. I stick with the brand. Period.