
When you’ve been seizure-free for years, the last thing you want is for your pharmacy to switch your medication without telling you. Yet that’s exactly what happens to thousands of people taking antiseizure medications (ASMs) every year - not because of a mistake, but because of a policy meant to save money. Generic substitution sounds simple: same active ingredient, lower price. But for drugs with a narrow therapeutic index, like many antiseizure medications, that small difference in how the body absorbs the drug can mean the difference between safety and a life-threatening seizure.
Why Antiseizure Medications Are Different
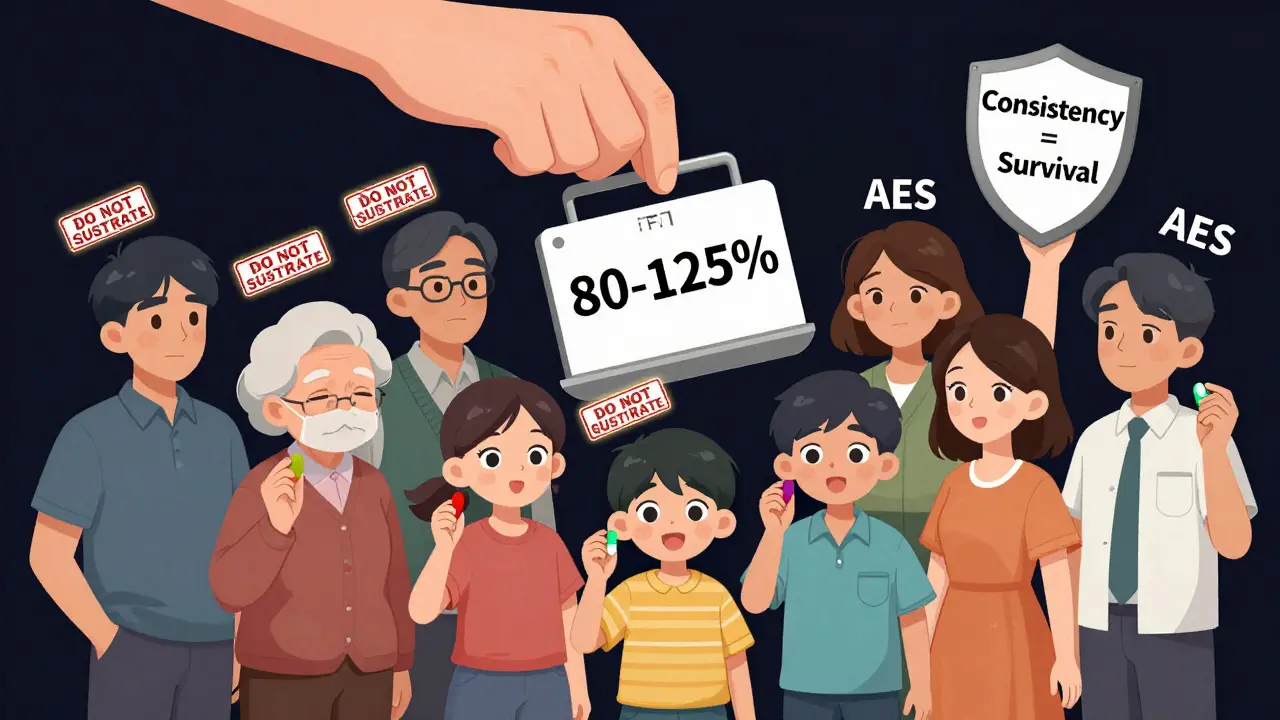
Not all medications are created equal when it comes to switching brands. Most drugs - like antibiotics or blood pressure pills - can be swapped between generic and brand versions without issue. But antiseizure drugs are in a class of their own. Many of them, including lamotrigine, carbamazepine, and valproic acid, have a narrow therapeutic index. That means the gap between a dose that works and one that causes harm is tiny. A 15% drop in blood levels might trigger a seizure. A 15% increase could cause dizziness, confusion, or even liver damage. The FDA says generics are bioequivalent if their absorption falls within 80-125% of the brand-name drug. That sounds precise. But for epilepsy patients, that 45% range is enormous. Imagine your blood level needs to stay between 5 and 7 micrograms per milliliter. A generic that puts you at 4.8? You’re now outside the safe zone. And it’s not just about the active ingredient. Fillers, coatings, and release mechanisms can change how quickly the drug enters your system. A generic version of extended-release lamotrigine might release the drug faster than the brand, causing spikes and crashes in your bloodstream - even if the total amount absorbed is technically "equivalent."The Real Cost of Saving Money
It’s true: generics cost 30-80% less. In the U.S., they make up about 90% of all antiseizure prescriptions. But the savings aren’t always clear-cut. A 2008 study published in Neurology found that switching to generic lamotrigine led to a 23% increase in doctor visits and an 18% rise in hospitalizations. Why? Because when seizures return, the cost of emergency care, missed work, and lost productivity often outweighs the drug savings. A global survey of 1,247 healthcare professionals in 68 countries found that 40% had seen patients experience more seizures after switching to generics. Another 17% reported more side effects. These aren’t rare cases. They’re patterns. And they’re backed by patient stories. One person on the Epilepsy Foundation’s forum wrote: "I’d been seizure-free for five years. After my pharmacy switched me to generic Lamictal, I had three seizures in two weeks." Another Reddit user said switching between different generic versions - each with different colors and shapes - made them anxious enough to trigger their first seizure in two years.What the Experts Say
There’s a deep divide between regulators and clinicians. The FDA maintains that generic substitution doesn’t increase risk. But neurologists who treat epilepsy daily see something else. Dr. Philip Glass from Montefiore Medical Center says, "The evidence is clear that for narrow therapeutic index drugs like many ASMs, even small variations matter." His center’s policy? Never switch patients with difficult-to-control epilepsy unless absolutely necessary. The American Epilepsy Society (AES) takes a middle ground. They agree the FDA’s bioequivalence standards are scientifically sound - but they also urge caution. Their 2018 position statement says: "Heightened caution is needed for medically complex patients." That includes people with frequent seizures, cognitive issues, or anxiety disorders. For them, even the stress of changing pill appearance can be a seizure trigger. In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) is even clearer: "Consistency of supply is important where the consequence of therapeutic failure might have serious clinical consequences." That’s not a vague suggestion. It’s a warning.
Who’s Most at Risk?
Not everyone needs to avoid generics. But some groups are far more vulnerable:- People with frequent or uncontrolled seizures
- Those taking multiple antiseizure drugs (polypharmacy)
- Patients with memory problems or cognitive decline
- Children and elderly individuals who rely on caregivers
- People on the ketogenic diet - some generic fillers contain hidden carbs
- Anyone who’s been stable for months or years
What You Can Do
You don’t have to accept random switches. Here’s how to protect yourself:- Ask your neurologist to write "Dispense as Written" or "Do Not Substitute" on your prescription. This legally prevents the pharmacy from switching without your doctor’s approval.
- Check your pills every time. If the color, shape, or imprint changes, call your pharmacy. Ask if it’s the same version you’ve been taking. If not, ask them to refill with your original brand or generic.
- Keep a seizure diary. Note any changes in frequency, severity, or side effects after a switch. This data helps your doctor decide if the change caused the problem.
- Know your medication’s name. Don’t just say "my seizure medicine." Know if you’re on lamotrigine, carbamazepine, or valproic acid - and whether it’s brand or generic.
- Use the same pharmacy. Chain pharmacies often switch generics based on cost. Independent pharmacies are more likely to hold your preferred version in stock.
What Doctors and Pharmacies Should Do
Many neurologists say they weren’t trained on bioequivalence in medical school. A 2022 survey found that 78% of neurologists felt underprepared to advise patients on generic substitution. That needs to change. Pharmacists, too, need better guidance. While they’re trained to fill prescriptions, few are taught how to recognize when a switch might be dangerous. The AES and Epilepsy Foundation offer free education modules - but uptake is low. More training, clearer labeling, and standardized communication between prescribers, pharmacists, and patients are essential.The Bigger Picture
The global antiseizure medication market is worth over $6 billion. Generics dominate it - and will keep growing. But the push for cost-cutting can’t ignore patient safety. The FDA is now considering tighter bioequivalence standards for narrow therapeutic index drugs - possibly narrowing the acceptable range from 80-125% to 90-111%. That’s a step in the right direction. Meanwhile, newer ASMs like cenobamate and fenfluramine have complex absorption profiles. These aren’t the old, simple drugs. They’re precision tools. And precision medicine demands consistency.Final Thoughts
Generic substitution isn’t bad. It’s necessary for access. But it shouldn’t be automatic - especially for antiseizure drugs. For people living with epilepsy, stability isn’t a luxury. It’s survival. If you’ve been doing well, don’t let a pharmacy change your medication without your knowledge. Speak up. Ask questions. Demand consistency. Your brain deserves nothing less.11 Comments
Write a comment
More Articles

Buy Cheap Generic Crestor Online - Affordable Cholesterol Medication
Learn how to safely buy cheap generic Crestor online, compare prices, verify legitimate UK pharmacies, and avoid scams while saving on cholesterol medication.

The Importance of Self-Care for Breast Cancer Survivors
As a breast cancer survivor, I cannot stress enough the importance of self-care in our journey to recovery. Taking care of our physical, emotional, and mental well-being is crucial in helping us regain our strength and confidence. By engaging in regular exercise, maintaining a healthy diet, and seeking emotional support, we can significantly improve our overall health and reduce the risk of recurrence. Surrounding ourselves with positive influences and seeking professional help when needed also plays a vital role in our healing process. Remember, self-care is not selfish; it is an essential part of our journey to becoming strong, resilient survivors.

Terry Free
December 26, 2025 AT 02:55So let me get this straight - we’re letting pharmacies play Russian roulette with people’s brains because a pill costs $5 less? The FDA’s 80-125% bioequivalence window isn’t science, it’s a corporate loophole dressed up as regulation. If your blood level dips 15% below therapeutic and you seize, is that a ‘pharmaco-economic win’? I’ve seen patients go from zero seizures to three in a week after a generic switch. This isn’t about cost. It’s about negligence disguised as efficiency.
And don’t give me that ‘same active ingredient’ nonsense. Fillers matter. Coatings matter. Release kinetics matter. You wouldn’t swap a Ferrari engine for a ‘bioequivalent’ Honda block and call it the same car. Why do we accept this with brain drugs?
Doctors need to start writing ‘Dispense as Written’ like it’s a life-or-death order - because it is. And pharmacies? They need training, not just profit margins.
Meanwhile, the Epilepsy Foundation’s data is screaming. 27% of patients switched back. That’s not anecdotal. That’s a systemic failure.
Generic substitution is fine for ibuprofen. Not for lamotrigine. Not for carbamazepine. Not for anyone whose brain depends on stability, not savings.