
Anticoagulant Dental Procedure Risk Calculator
Assess Your Dental Procedure Risk
This tool helps you understand bleeding risks when having dental work while on anticoagulants. Based on your medication type and procedure, it will provide evidence-based guidance.
When you're on blood thinners, even a simple dental cleaning can feel risky. You’ve heard the warnings: anticoagulants increase bleeding. But what if stopping them is even more dangerous? This isn’t just about a little extra bleeding after a tooth extraction-it’s about preventing strokes, heart attacks, and blood clots that can kill you. Millions of people take anticoagulants for atrial fibrillation, artificial heart valves, or deep vein thrombosis. And more of them are walking into dental offices than ever before. The good news? You don’t need to stop your medication for most procedures. The key is knowing how to manage it right.
Why Stopping Blood Thinners Is Often the Bigger Risk
For years, dentists and patients assumed the safest move was to pause blood thinners before any dental work. That’s what doctors used to do with warfarin. But research from the last decade flipped that thinking. A 2020 JAMA Internal Medicine study of over 3,000 patients found that stopping anticoagulants for dental procedures increased the risk of stroke by 3.5 times. For someone with a mechanical heart valve or chronic atrial fibrillation, a stroke isn’t just a scary word-it’s often fatal or permanently disabling. Dental bleeding, on the other hand, is usually minor and controllable. One expert put it bluntly: thromboembolic events carry 10 to 20 times higher mortality than bleeding from a tooth extraction.What Counts as a Low-Risk Dental Procedure?
Not all dental work is the same when you’re on blood thinners. The risk level depends on the procedure, not just the drug. Low-risk procedures include:- Single tooth extractions
- Simple fillings
- Scaling and root planing (deep cleaning)
- Local anesthesia injections
- Periodontal probing
What About Higher-Risk Procedures?
Some dental work carries more bleeding risk. These include:- Multiple tooth extractions
- Periodontal surgery
- Implant placements (especially more than two)
- Full-mouth extractions
Warfarin vs. DOACs: What’s the Difference?
There are two main types of blood thinners: warfarin and direct oral anticoagulants (DOACs). Warfarin has been around for decades. It requires regular INR blood tests to make sure your blood isn’t too thin or too thick. DOACs-like apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa)-don’t need routine testing. They’re more predictable, but they’re not risk-free. A 2022 meta-analysis of over 14,000 patients found warfarin has a 2.3-fold higher bleeding risk during dental procedures than DOACs. But DOACs aren’t perfect. Rivaroxaban carries a higher chance of stomach bleeding than warfarin. Edoxaban can interact badly with proton pump inhibitors like omeprazole, which many patients take for heartburn. That interaction can raise bleeding risk by 2.4 times. That’s a hidden trap for implant patients who need bone healing and are also on acid-reducing meds.
How Dentists Control Bleeding Without Stopping Your Meds
You don’t need to stop your blood thinner. But your dentist needs tools to control bleeding. Here’s what works:- Tranexamic acid mouthwash (5%)-used four times a day for a week-cuts bleeding risk by 62%. It’s cheap, safe, and effective.
- Oxidized regenerated cellulose (Surgicel®)-a dissolvable sponge placed in the socket-reduces bleeding time by 47% compared to plain gauze.
- Microfibrillar collagen (Avitene®)-a natural hemostatic agent-stops bleeding in 92.3% of cases in anticoagulated patients.
- Lidocaine with epinephrine (1:100,000)-the local anesthetic-constricts blood vessels and reduces bleeding by 32% compared to plain lidocaine.
What About Painkillers and Antibiotics?
Pain management is where things get tricky. NSAIDs like ibuprofen, naproxen, or aspirin (even low-dose) can double or triple your bleeding risk when combined with anticoagulants. The answer? Stick with acetaminophen (paracetamol). But even that has a catch: if you take more than 2 grams a day for over seven days, it can raise your INR. Monitor it. Antibiotics matter too. Metronidazole (Flagyl) can boost warfarin’s effect by 33-50%, leading to dangerous INR spikes. Azithromycin? No interaction. Always tell your dentist what antibiotics you’re on-or might be prescribed.What No One Tells You About Bridging
Some doctors still recommend “bridging”-switching from warfarin to heparin shots before surgery, then switching back. It sounds smart. But it’s not. The 2015 BRIDGE trial, published in the New England Journal of Medicine, showed bridging triples major bleeding risk (3.2% vs 1.1%) without reducing clots. The American College of Cardiology says it’s never justified for dental work. If your doctor suggests it, ask for the evidence. Most likely, they’re operating on old habits.
Common Mistakes Dentists Still Make
Despite clear guidelines, mistakes are common. A 2022 survey of 1,247 U.S. dentists found 43.7% still stop warfarin for single extractions. That’s against every major guideline. And the consequences? In 18.3% of those cases, patients ended up in the emergency room within 30 days with a stroke or clot. The problem isn’t lack of knowledge-it’s lack of systems. Clinics that use checklists cut adverse events by 67%. A simple form that asks: “Last INR date? INR value? Last DOAC dose? Hemostatic plan?” makes all the difference.What’s New in 2025?
Technology is helping. Portable INR devices like CoaguChek® let dentists check your blood thinning level in under a minute. No more waiting for lab results. In 2023, the FDA updated approval for andexanet alfa (Andexxa®), a reversal agent for DOACs. It’s expensive-$18,850 per vial-but it can save lives in emergencies. Emerging research is testing topical gels with recombinant factor VIIa. Early trials show they cut bleeding time by over 60%. And AI tools are being developed to predict bleeding risk with 89% accuracy by analyzing 17 factors: your INR, platelet count, procedure type, age, kidney function, and more.What You Should Do Before Your Appointment
Don’t wait for your dentist to ask. Take charge:- Bring a list of every medication you take, including doses and timing.
- Know your latest INR value (if on warfarin) and when it was tested.
- Know the name and dose of your DOAC, and when you last took it.
- Ask: “Will I need to stop my blood thinner? What hemostatic measures will you use?”
- Ask for tranexamic acid mouthwash if it’s not offered.
- Never take NSAIDs for pain after the procedure-use acetaminophen instead.
Final Thought: It’s About Balance, Not Fear
Blood thinners aren’t the enemy. Stopping them without reason is. Dental care is essential. Skipping cleanings or delaying extractions because you’re scared of bleeding can lead to infections, tooth loss, and worse-systemic inflammation that increases your heart risk. With the right protocols, you can get the care you need without putting your life on the line. The science is clear. The tools are available. The only thing missing is confidence-yours and your dentist’s.Should I stop my blood thinner before a tooth extraction?
No, for most single extractions and routine procedures, you should continue your blood thinner. Stopping it increases your risk of stroke or clot by 3.5 times, according to JAMA Internal Medicine. Bleeding from a tooth extraction is usually minor and can be controlled with proper techniques like tranexamic acid mouthwash or Surgicel®. Only stop your medication if your cardiologist or hematologist specifically advises it for a high-risk procedure.
What if I take rivaroxaban or Eliquis? Do I need to wait after my last dose?
Yes. For once-daily DOACs like rivaroxaban, wait at least 12-24 hours after your last dose before a procedure. For twice-daily drugs like apixaban, wait 24-48 hours. If you take your morning dose and have an afternoon appointment, reschedule. Studies show extractions done less than 4 hours after rivaroxaban have an 8.7% major bleeding rate-compared to 1.2% if you wait longer. Timing matters more than INR with DOACs.
Can I take ibuprofen for pain after a dental procedure?
No. Ibuprofen, naproxen, and other NSAIDs increase bleeding risk 3 to 6 times when combined with anticoagulants. Use acetaminophen (paracetamol) instead. But if you take more than 2 grams a day for over seven days, it can affect your INR. Stick to the lowest effective dose for the shortest time.
Do I need an INR test before every dental visit?
Only if you’re on warfarin and having a moderate- or high-risk procedure. For low-risk procedures like fillings or single extractions, an INR within the last 72 hours is sufficient. If your last test was over a week ago, ask your doctor for a quick check. For DOACs, no INR test is needed-but you must know when you last took your dose.
Is it safe to get dental implants if I’m on blood thinners?
Yes, but it’s higher risk. Implants require multiple surgical steps and bone healing. For one or two implants, continue your anticoagulant with INR under 2.5 (if on warfarin) and use hemostatic agents like collagen or tranexamic acid. For three or more implants, consult your hematologist. Some may recommend a temporary INR target of 2.0. Avoid bridging with heparin-it increases bleeding without benefit.
15 Comments
Write a comment
More Articles
Prescriber Attitudes Toward NTI Drugs and Substitution
Prescribers remain cautious about substituting generic versions of narrow therapeutic index (NTI) drugs due to safety concerns, despite FDA assurances. Real-world data, state laws, and clinical experience shape ongoing debates over substitution practices.

Rising Threat of Candidemia and Disseminated Candida Infections in Hospitals
Explore why candidemia and disseminated Candida infections are rising in hospitals, learn to identify at‑risk patients, diagnose quickly, treat effectively, and prevent outbreaks with proven strategies.
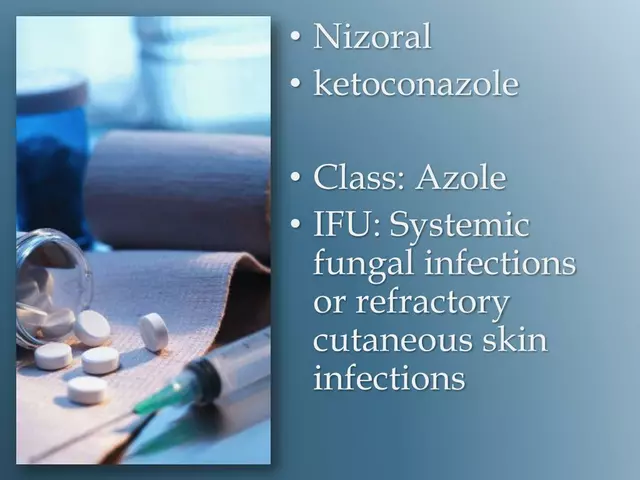
Tips for preventing fungal infections and the need for ketoconazole treatment
In my latest blog, I've shared some handy tips for preventing fungal infections so you can potentially avoid the need for treatments like ketoconazole. We dive into the importance of maintaining good hygiene, keeping your skin dry and clean, and wearing breathable fabrics to prevent a conducive environment for fungi. We also touch on the importance of a healthy diet to boost your immune system. If you do get an infection, don't panic because treatments like ketoconazole are there to help. But remember, prevention is always better than cure!
Desmond Khoo
December 8, 2025 AT 01:53OMG this is LIFE-SAVING info!! 🙌 I was terrified to get my wisdom teeth out on Eliquis, but now I feel like a superhero. Tranexamic acid mouthwash? I’m grabbing some today. Dentists need to stop acting like we’re all gonna bleed out. 💪🦷