
When you buy a pill, a medical device, or even a simple health product, you assume it’s safe. But what if the factory that made it didn’t follow the same rules as your country’s standards? That’s not a hypothetical. In 2024, foreign manufacturing quality failures caused 37% of all drug shortages in the U.S., according to FDA data. And it’s getting worse.
Why Overseas Production Is Riskier Than Ever
For years, companies moved production overseas to save money. Labor costs in China, India, and Vietnam were a third of what they were in the U.S. or Europe. But the savings came with hidden dangers. What looked like a cost-cutting move turned into a ticking time bomb. In 2025, the situation isn’t just about bad batches or sloppy workers. It’s about systemic breakdowns. A factory in Wuhu, China, was caught in February 2025 for letting impurities in pharmaceuticals that violated U.S. standards. The FDA issued a warning letter - but that’s not rare. Nearly half of all Chinese drug manufacturing sites received FDA Form 483 notices in 2024 - the official red flag for violations. In comparison, only 29% of U.S. sites did. The problem isn’t just China. Indian facilities accounted for 34% of all FDA drug import alerts in 2024, even though they only make up 25% of foreign production. Meanwhile, Vietnamese factories have improved - up 18% in quality metrics since 2022 - but they’re still catching up. And here’s the kicker: most inspections in China are announced in advance. The FDA tells the factory when they’re coming. That means companies have time to clean up, hide problems, or even swap out bad batches. In the U.S., 95% of inspections are unannounced. In China? Only 22% were in 2024. That’s not oversight - it’s a loophole.The Hidden Costs of Bad Quality
You think you’re saving money by making things overseas? Think again. When a batch of pills is contaminated, or a medical device fails in the field, the real cost explodes. Rework. Recalls. Legal fees. Lost trust. FDA fines. A single recall can cost millions. Harris Sliwoski’s analysis shows unaddressed quality issues add 15-25% to total manufacturing costs - more than the labor savings you thought you were getting. One company in Minnesota learned this the hard way. They imported a line of medical devices from Shenzhen. The supplier claimed they used medical-grade silicone. They didn’t. They used industrial-grade material - cheaper, but toxic when implanted. 12,000 units were recalled. The company lost $2.3 million. They also lost their reputation. Patients stopped trusting their brand. And it’s not just financial. In 2024, 62% of all drug recalls in the U.S. came from foreign facilities - even though those facilities only produced 43% of the total volume. That means foreign-made drugs are more than 40% more likely to be pulled from shelves than U.S.-made ones.What’s Going Wrong Inside the Factories
It’s not always fraud. Sometimes it’s just bad systems. The most common failures? Material substitution. That’s when a factory swaps out expensive, regulated materials for cheaper, unapproved ones. Brookings found this happens in 68% of inspected Chinese facilities. In one case, a supplier replaced sterile packaging with non-sterile - and no one noticed until patients got infections. Then there’s inadequate process validation. That’s when a factory doesn’t prove their process consistently produces safe products. It happened in 42% of non-compliant sites. They just guess it works. And falsified documentation? That’s the most dangerous. 29% of inspected sites were caught lying on reports - changing test results, forging signatures, or inventing quality checks that never happened. One factory in India was found to have backdated batch records for six months. The FDA didn’t catch it until a whistleblower came forward.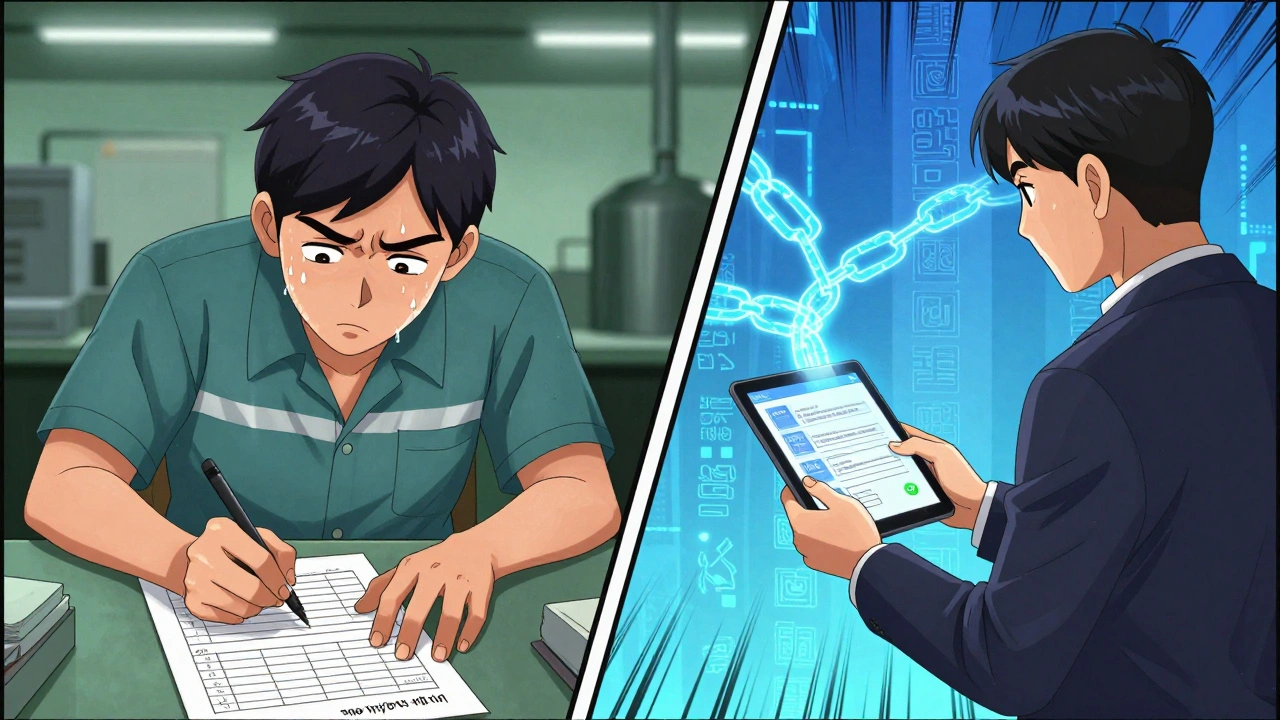
Why AI Isn’t Fixing It - Yet
You’d think technology would solve this. AI-powered visual inspection systems can spot defects with 99.2% accuracy - better than any human. But only 22% of Chinese manufacturers use them. Why? Because it’s expensive. And many factories are barely surviving. When margins are thin, investing in AI feels like a luxury. Instead, they cut corners. They hire undertrained staff. They skip calibration. They ignore maintenance logs. Deloitte’s 2025 report found that companies with full digital quality ecosystems - AI, IoT sensors, blockchain traceability - have 33% fewer defects. But those companies are the exception. Most are still using clipboards and handwritten logs.What Works: The Few That Got It Right
There are success stories. But they’re rare - and they didn’t happen by accident. One medical device company in Minnesota fixed their quality problems with a “China-specific quality triad.” First, they hired a full-time quality manager in Shenzhen - not a middleman, not a translator, but someone with real authority. Second, they used blockchain to track every component from raw material to final product. Third, they hired an independent third-party auditor to show up unannounced every month. Result? Defects dropped from 12.7% to 0.8% in two years. Another company in Germany started requiring mandatory pre-shipment testing - not just at the factory, but at a certified lab in Germany before the goods even left China. It added $15 per unit to cost. But it stopped three major recalls in 18 months. These companies didn’t rely on trust. They built systems that couldn’t be fooled.The Regulatory Shift: What’s Changing in 2025
The FDA is finally catching up. In May 2025, Commissioner Marty Makary announced a major shift: unannounced inspections will rise to 40% of all foreign inspections by the end of 2025 - and hit 75% by 2027. That’s huge. No more warning calls. No more cleaning up before inspectors arrive. It’s a direct response to the “double standard” that let bad actors hide for years. President Trump’s May 2025 executive order also raised user fees for foreign manufacturers. Compliance costs are expected to jump 18-25%. That will push out the weakest suppliers - the ones cutting corners just to survive. Meanwhile, the EU’s Qualified Person (QP) system is getting attention. In Europe, every batch of medicine must be signed off by a certified professional who takes personal legal responsibility. That’s not a formality - it’s a liability. And it’s working. EU-manufactured drugs have 22% fewer quality failures than imports from non-EU countries. Experts like Dr. Jessica Rose from White & Case are pushing for a similar U.S. system. One person, with a license, accountable for every batch. No more hiding behind “the supplier did it.”
What You Need to Do Now
If you’re importing products - especially medicines, medical devices, or health-related goods - here’s what you must do:- Don’t trust certifications alone. ISO 9001 doesn’t guarantee quality. It guarantees paperwork. Verify with on-site audits.
- Insist on unannounced audits. Make it a contract requirement. No exceptions.
- Hire local quality staff. Not agents. Not middlemen. Someone on the ground with real authority and access to the production line.
- Test before shipment. Use a third-party lab in your country to test random batches. Don’t rely on the factory’s lab.
- Use blockchain or digital traceability. Even basic systems that track raw material sources and batch numbers cut fraud by 60%.
- Train your team. Spend $18,500 per year per facility on quality training. It’s not an expense - it’s insurance.
The Bigger Picture: Friend-Shoring and the New Supply Chain
More companies are moving production to allied countries - Mexico, Poland, India, Vietnam. It’s called “friend-shoring.” But it’s not a magic fix. New suppliers mean new risks. New regulations. New quality gaps. Many of these countries don’t have the infrastructure to handle high-volume, high-precision manufacturing yet. China’s share of global manufacturing dropped from 33.2% in 2022 to 31.6% in 2025. But that doesn’t mean it’s safer. The market is splitting. On one side, high-end “Made in China 2025” factories are investing in automation and AI. On the other, thousands of small suppliers are collapsing under debt, cutting corners just to stay open. The risk isn’t going away. It’s just changing shape.Final Reality Check
Overseas manufacturing isn’t evil. It’s not inherently dangerous. But it’s not safe either. It’s a system that rewards speed and cost - not quality or transparency. The companies that survive 2025 and beyond aren’t the ones who saved the most on labor. They’re the ones who invested the most in control. If you’re still relying on trust, you’re already behind. If you’re still using vague contracts with “reasonable quality” as a standard, you’re asking for trouble. Harris Sliwoski found 58% of recoverable losses came from vague quality clauses. The next recall, the next lawsuit, the next patient injury - it won’t be an accident. It’ll be the result of a decision you made months or years ago. You can’t outsource quality. You can only manage it - with systems, not hope.14 Comments
Write a comment
More Articles

Germanium Supplements: Health Benefits, Safety Risks, and Evidence‑Based Alternatives (2025 Guide)
Curious about germanium supplements? Get clear facts on claimed benefits, real risks, UK context, and safer alternatives-so you can choose wisely in 2025.

Ginkgo Biloba and Blood Thinners: What You Need to Know About Bleeding Risk
Ginkgo biloba may seem harmless, but when mixed with blood thinners like aspirin or warfarin, it can cause dangerous bleeding. Learn who's at risk, which meds to avoid, and what to do before surgery.

Foreign Manufacturing Quality Issues: How Overseas Production Risks Are Rising in 2025
Foreign manufacturing quality issues are worsening in 2025, with rising FDA drug recalls, material fraud, and unannounced inspections. Learn how overseas production risks affect health products and what companies must do to stay compliant and safe.
Gerald Nauschnegg
December 3, 2025 AT 22:40Let me tell you something - I work in pharma procurement and I’ve seen this firsthand. Factories in China don’t just cut corners, they bulldoze the whole damn building. I had a supplier once swear their sterile packaging met ISO standards. Turned out they reused autoclave bags three times. No one checked until a kid got sepsis from a syringe. That’s not negligence. That’s criminal.
And don’t get me started on the ‘pre-announced inspections.’ It’s like letting a thief clean the house before the police show up. The FDA knows this. They just don’t have the budget to fix it. So we pay the price in recalls and deaths.
And yet, CEOs still sign off on these deals because the quarterly report looks better. Profit over people. Again. Always again.