Every year, over 150,000 people in the U.S. end up in the emergency room because something they ate made their medication work too well-or not at all. It’s not rare. It’s not exotic. It’s happening to people just like you, taking their pills with breakfast, snacking on nuts, or sipping grapefruit juice with their statin. And most of them had no idea.
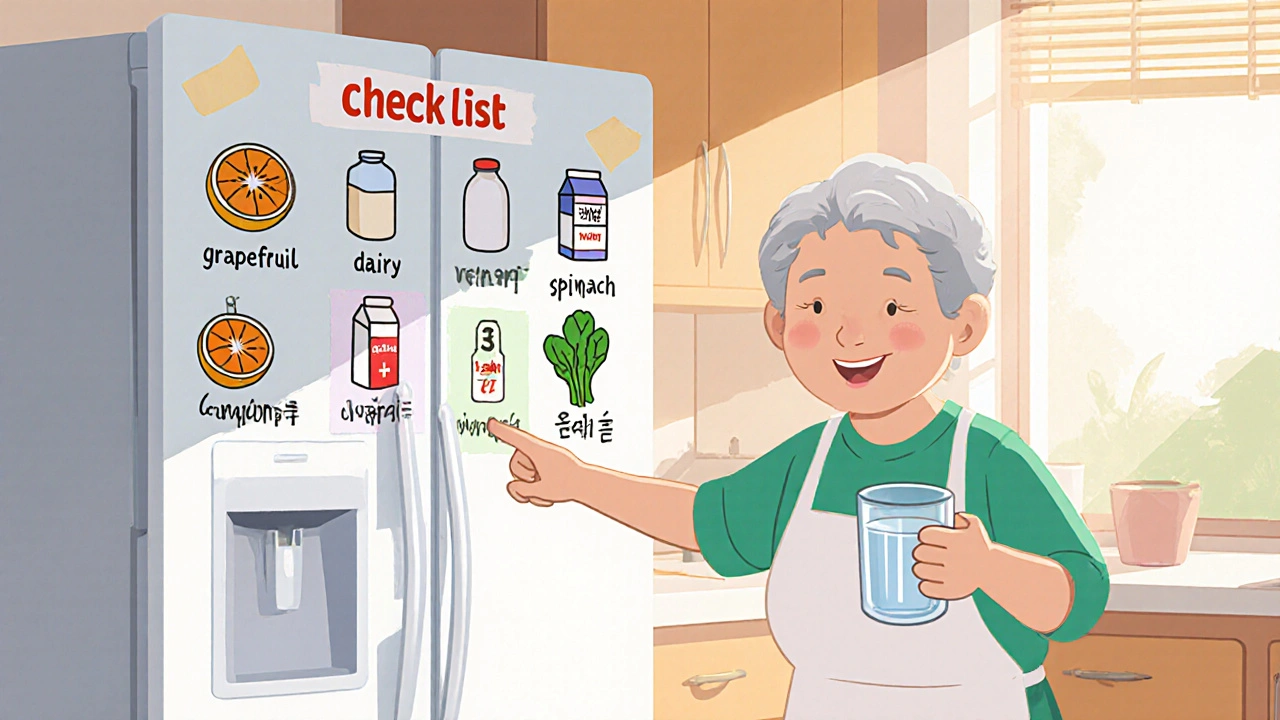
You don’t need a pharmacy degree to protect yourself. You just need a simple, clear checklist you can keep on your fridge. This isn’t about memorizing complex science. It’s about writing down what you take, what you eat, and what happens when they meet.
Why This Checklist Matters
Medications aren’t just chemicals floating in your body. They react with food, drinks, even supplements like magnesium or St. John’s wort. Some interactions are mild-maybe your stomach feels off. Others are life-threatening. Warfarin, for example, can turn deadly if you suddenly eat a big salad one day and none the next. Grapefruit juice can make your blood pressure medication 500% stronger. That’s not a rumor. That’s FDA data.
The problem isn’t that doctors forget to warn you. It’s that you forget what they said. Or you didn’t know to ask. Or your meds changed, but your list didn’t. According to the American Heart Association, 68% of medication errors happen because the patient’s record was outdated. That’s why your checklist needs to be alive-not a one-time form you fill out and forget.
What Goes on the Checklist
Start with everything you take. Not just prescriptions. Include over-the-counter pills, vitamins, herbal teas, and supplements. If you take it regularly, it belongs on the list.
For each item, write down:
- Drug name (both brand and generic, like warfarin or Coumadin)
- Dosage (e.g., 5 mg once daily)
- Purpose (e.g., prevents blood clots)
- Time taken (e.g., 8 AM with water)
- Prescriber (e.g., Dr. Sarah Chen, Cardiology Associates)
Now, for each medication, note the food or drink it interacts with. Don’t guess. Use reliable sources: the FDA’s medication guides, the New Zealand Formulary, or your pharmacist’s printed interaction sheet. Write it clearly:
- High Risk - Avoid completely. Example: Grapefruit juice with simvastatin - can cause muscle damage.
- Moderate Risk - Separate by time. Example: Dairy with ciprofloxacin - wait 2 hours after taking pill.
- Low Risk - Monitor. Example: Leafy greens with warfarin - eat the same amount daily.
Be specific. Don’t write “avoid greens.” Write: 1 cup raw spinach, ½ cup cooked kale - keep daily intake consistent. Why? Because cooked spinach has 70% less vitamin K than raw. That matters.
How to Research Interactions
You don’t need to be a scientist. But you do need to use trusted sources. Here’s where to look:
- FDA Drug Safety Communications - Search for your drug name + “food interaction” on fda.gov. They update these regularly.
- New Zealand Formulary Interaction Checker - Free, reliable, and used by pharmacists worldwide. Type in your drug and it lists foods to avoid.
- SEFH Drug-Food/Herb Interaction Guide - A laminated card you can stick on your fridge. Color-coded. Easy to read.
- Your pharmacist - Ask them to review your list. Most will do it for free during a refill.
Never rely on Google or random apps. A 2024 FDA report found that 62% of unregulated AI health apps give wrong interaction advice. Stick to official sources.

Choose Your Format: Paper or Digital?
There’s no one-size-fits-all. It’s about what works for you.
Paper checklist - Best if you’re older, don’t use tech often, or live in a place with spotty internet. Use the FDA’s free “My Medicines” PDF template. Print it, fill it out with a pen, and tape it to the fridge. It’s visible. It’s simple. It doesn’t need charging. And in an emergency, paramedics can see it instantly.
Digital checklist - Apps like Medisafe or MyTherapy can remind you when to take pills and flag new interactions automatically. They’re great if you take five or more meds. But they require a smartphone, regular updates, and internet access. If your phone dies, your checklist dies too.
Most people over 75 use paper. Most under 60 use apps. But here’s the smart move: keep both. Use the app for reminders and the paper one as your backup. That way, you’re covered no matter what.
Keep It Updated
Your checklist is useless if it’s outdated. And most people let it rot.
Set a rule: update it every time your meds change. That means:
- When your doctor adds, removes, or changes a dose
- When you start a new supplement (even “natural” ones)
- When you switch brands (e.g., from generic lisinopril to brand-name Zestril)
Also, update it every month. Pick a day-say, the 1st of the month-when you refill your prescriptions. Use that day to review your list. Ask yourself: “Did anything change?” If yes, update it. If no, write the date: Last updated: November 1, 2025.
According to a 2023 FDA analysis, 28% of checklist-related errors happened because the list wasn’t updated after a medication change. Don’t be that person.
Where to Keep It
Out of sight = out of mind. That’s why 82% of people who keep their checklist on the fridge report fewer mistakes.
Put it where you see it every day:
- On the fridge (best spot - near your meals)
- Inside your medicine cabinet (next to your pills)
- In your wallet or purse (for emergencies)
- Give a copy to a family member or caregiver
Use color coding. Red for high-risk. Yellow for moderate. Green for low. It takes seconds to add a highlighter, but it saves minutes-and possibly your life-when you’re in a hurry.

When to Talk to Your Doctor or Pharmacist
Bring your checklist to every appointment. Not just when you’re sick. Bring it to your annual check-up. Bring it when you refill your meds. Say: “I made this to keep myself safe. Can you check it?”
Pharmacists are trained to catch these things. In fact, Medicare Advantage plans now pay for Medication Therapy Management sessions-where a pharmacist reviews your list, food habits, and supplements. It’s free. Use it.
If you’re on warfarin, you must track vitamin K intake daily. If you’re on MAO inhibitors, you must avoid aged cheeses, cured meats, and tap beer. These aren’t suggestions. They’re medical rules. And your checklist is your shield.
Real Stories, Real Results
One man in Ohio took tacrolimus after a kidney transplant. He drank grapefruit juice every morning. His levels spiked. He nearly lost the transplant. He didn’t know about the interaction until his pharmacist flagged it after he brought his checklist.
A woman in Florida took amiodarone for her heart. She ate a lot of kale. Her doctor didn’t mention the interaction. She ended up in the ER with dangerously low blood pressure. She started her checklist. Now she eats one cup of cooked kale every Tuesday. No more surprises.
These aren’t rare cases. They’re common. And they’re preventable.
Start Today
You don’t need to be perfect. You just need to start.
Right now, gather every pill bottle, supplement box, and prescription label. Lay them out on your kitchen table. Grab a pen and paper. Write down each one. Look up one interaction-just one. Maybe grapefruit and your statin. Or dairy and your antibiotic.
Put it on the fridge. Update it next month. Show it to your pharmacist.
This isn’t about control. It’s about safety. You’re not just taking pills. You’re managing your health. And this checklist? It’s the simplest, most powerful tool you have to stay in control.
What foods commonly interact with medications?
Common culprits include grapefruit juice (interacts with statins, blood pressure meds, and immunosuppressants), dairy products (blocks absorption of antibiotics like ciprofloxacin), leafy greens high in vitamin K (affect warfarin), aged cheeses and cured meats (dangerous with MAO inhibitors), and alcohol (can increase sedation or liver damage with painkillers and antidepressants).
Can I just rely on my pharmacist to warn me?
Pharmacists do their best, but they don’t know your full diet or habits unless you tell them. A 2024 study found that patients who brought their own food-medication checklist to the pharmacy had 65% fewer errors than those who didn’t. Your checklist gives your pharmacist the full picture.
Is it safe to skip a food interaction if I only eat it once in a while?
No. Even occasional consumption can be risky. For example, eating grapefruit once while on simvastatin can raise drug levels enough to cause muscle damage. With warfarin, one big salad can throw off your INR levels for days. Consistency matters more than frequency.
Do herbal supplements count as food interactions?
Yes. Supplements like St. John’s wort, garlic, ginkgo, and ginseng can interfere with blood thinners, antidepressants, and heart medications. They’re not regulated like drugs, so their effects are unpredictable. Always list them on your checklist.
What if I don’t have a printer or smartphone?
Use pen and paper. Write your list on a piece of notebook paper. Tape it to your fridge. You don’t need tech to stay safe. The simplest checklist is the one you actually use. Many seniors use handwritten lists-and they work.
How often should I review my checklist?
Update it every time your medications change. Also, review it every month-ideally when you refill your prescriptions. Write the date each time you update it. This prevents the 28% of errors caused by outdated information.
14 Comments
Write a comment
More Articles

How to Build a Shared Medication Calendar for Family and Caregiver Coordination
Learn how to build a shared medication calendar that keeps your loved one safe, reduces caregiver stress, and prevents dangerous drug interactions with family and professional caregivers.

Kathryn Ware
November 17, 2025 AT 09:53OMG I JUST REALIZED I’VE BEEN DRINKING GRAPEFRUIT JUICE WITH MY STATIN FOR YEARS 😱 I thought it was ‘healthy’ lol. Thanks for this-I printed the checklist and taped it to my fridge next to my coffee mugs. Also, I’m now calling my pharmacist tomorrow to review my supplements. You just saved my liver, OP. 🙏💚