
NSAID Gastrointestinal Bleeding Risk Assessment
This tool helps you understand your risk of gastrointestinal bleeding while taking NSAIDs. Based on your answers, it will calculate your risk level and provide personalized recommendations.
Risk Factors Assessment
Answer the following questions to determine your risk level. Each 'yes' adds to your risk score.
Your Risk Assessment
You have risk factors.
Your Risk Factors:
Every year, millions of people reach for ibuprofen, naproxen, or aspirin to ease a headache, sore knee, or back pain. These drugs-called NSAIDs-are everywhere: on pharmacy shelves, in medicine cabinets, even in the pockets of older adults who take them daily. But behind the convenience lies a quiet danger: NSAIDs are one of the leading causes of gastrointestinal bleeding, especially in people with peptic ulcer disease. Many don’t realize they’re at risk until they’re in the hospital with black stools, dizziness, or a sudden drop in hemoglobin. This isn’t rare. It’s common. And it’s preventable.
How NSAIDs Cause Bleeding
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 is involved in inflammation and pain, which is why these drugs help. But COX-1 is the one that protects your stomach lining. It helps produce mucus and bicarbonate that shield your stomach and duodenum from acid. When NSAIDs shut down COX-1, that protective layer breaks down. The acid eats away at the tissue. What starts as a small erosion can turn into a deep ulcer-and sometimes, it bleeds.
This isn’t just about stomach ulcers. Bleeding can happen anywhere in the GI tract. A 1999 study from the Cleveland Clinic Journal of Medicine found that 86% of patients with lower GI bleeding had taken NSAIDs-even though they didn’t have a visible ulcer. That means you can bleed from the small intestine or colon without ever having a classic peptic ulcer. The damage is silent until it’s severe.
Grade 1 lesions are tiny surface scrapes. Grade 4 are deep ulcers with visible blood vessels. Once you hit Grade 3 or 4, bleeding becomes likely. And the risk isn’t the same for everyone. Age, other medications, and how much you take all change the game.
Who’s Most at Risk?
Not everyone who takes NSAIDs bleeds. But some people are walking into danger without knowing it. The biggest red flags:
- Age 70 or older-risk doubles every decade after 60
- History of peptic ulcer or prior GI bleeding
- Taking blood thinners like warfarin or aspirin
- Using corticosteroids (like prednisone)
- Taking more than one NSAID at a time
- Daily doses over 1,200 mg of ibuprofen
- Having serious heart, kidney, or liver disease
A 2021 American College of Gastroenterology guideline says if you have two or more of these, you’re in the high-risk group. That’s not a suggestion-it’s a warning. A 2017 Cochrane review showed that in high-risk patients, adding a proton pump inhibitor (PPI) like omeprazole cuts ulcer complications by 74%. That’s not a small win. It’s life-saving.
Over-the-Counter NSAIDs Are Just as Dangerous
Many people think, “It’s just Advil. It’s safe.” But that’s a myth. A 2021 review in Clinics in Medicine found that 26% of people take OTC NSAIDs at doses higher than recommended. And nearly half never tell their doctor. Why? Because they don’t see it as a drug. They see it as candy.
One Reddit user, u/ElderCareHelper, shared how their 78-year-old mother developed iron-deficiency anemia from slow, hidden bleeding. She had no pain, no nausea, no warning. Just fatigue and pale skin. Her hemoglobin dropped to 7.2 g/dL. She needed three units of blood. She’d been taking naproxen daily for arthritis for over a year. No one asked her about it.
That’s not an outlier. A 2022 Arthritis Foundation survey of over 5,000 people showed that 42% stopped taking NSAIDs because of stomach issues. But most didn’t stop because they were warned. They stopped because they got sick.

COX-2 Inhibitors: Safer for the Stomach, Riskier for the Heart
When the risks became too clear, drugmakers developed COX-2 inhibitors-drugs like celecoxib and rofecoxib-that targeted only the inflammation enzyme, sparing the stomach. And they worked. A 2000 Lancet study found celecoxib had half the rate of serious ulcers compared to ibuprofen.
But then came the catch. The 2004 APPROVe trial showed rofecoxib (Vioxx) doubled the risk of heart attacks. It was pulled from the market. Celecoxib stayed, but with a black box warning. Today, COX-2 inhibitors still carry a higher cardiovascular risk than traditional NSAIDs. For someone with heart disease, they might be worse than naproxen.
That’s why the American College of Rheumatology’s 2023 guidelines say: if you have heart problems, avoid COX-2 inhibitors. If you have a history of bleeding, use them with a PPI. There’s no perfect option. Only better trade-offs.
What Actually Protects Your Stomach?
If you need NSAIDs and you’re at risk, what can you do?
- PPIs (proton pump inhibitors): Omeprazole, esomeprazole, pantoprazole. These are the gold standard. They cut ulcer risk by 75%. They’re cheap, widely available, and well-tolerated.
- Misoprostol: This drug replaces the protective mucus that NSAIDs destroy. It works-but 1 in 5 people get diarrhea or cramps. Most quit taking it.
- H2 blockers: Like famotidine. They help a little, but not enough for high-risk patients.
- Combination drugs: Vimovo (naproxen + esomeprazole) was approved in 2023. In one trial, it cut ulcers from 25.6% to 7.3%. It’s more expensive, but for high-risk patients, it’s worth considering.
Don’t assume your doctor will bring this up. In a 2022 HealthUnlocked survey, 63% of NSAID users had GI symptoms-but only 37% talked to their doctor. If you’re taking NSAIDs daily and have any stomach discomfort, bloating, fatigue, or dark stools, say something. Don’t wait.
Real Numbers, Real Consequences
NSAID-related GI bleeding isn’t a footnote. It’s a public health crisis.
- 107,000 hospitalizations per year in the U.S.
- 16,500 deaths annually
- $2.2 billion in healthcare costs
That’s more than the entire annual budget of many small hospitals. And it’s almost entirely preventable. The FDA has required black box warnings on all NSAIDs since 2005. That’s the strongest warning they give. It’s not a suggestion. It’s a legal requirement because the data is undeniable.
And yet, the market keeps growing. The global NSAID market hit $11.3 billion in 2022. Nearly 1 in 6 U.S. adults takes them weekly. Among people with arthritis, it’s over 1 in 3. People need pain relief. But they also need protection.
What Should You Do?
If you’re on NSAIDs long-term:
- Ask yourself: Do I have any of the risk factors? Age? History of ulcers? Blood thinners? Steroids?
- If yes to two or more, talk to your doctor about a PPI. Don’t wait for symptoms.
- Use the lowest dose for the shortest time possible.
- Don’t mix NSAIDs. No ibuprofen + naproxen.
- Watch for signs: black or tarry stools, vomiting blood, unexplained fatigue, dizziness.
- Consider alternatives: acetaminophen for pain, physical therapy, weight loss, or topical treatments.
If you’re over 65 and taking NSAIDs without a PPI, you’re playing Russian roulette with your gut. The odds aren’t in your favor.
What’s Next?
Science is working on better options. New drugs called CINODs-COX-inhibiting nitric oxide donators-are in phase III trials. Naproxcinod, for example, showed 50% fewer ulcers than naproxen in a 2021 study. They might offer pain relief without the gut damage. But they’re years away.
For now, the best tools we have are simple: know your risk, use protection, and don’t assume OTC means safe. The goal isn’t to stop NSAIDs. It’s to use them wisely. Because pain matters. But so does your stomach.
8 Comments
Write a comment
More Articles

How to Create a Food and Medication Interaction Checklist at Home
Create a simple, personalized food and medication interaction checklist to prevent dangerous reactions. Learn what foods to avoid with common meds like warfarin and statins, how to update it, and where to keep it for maximum safety.
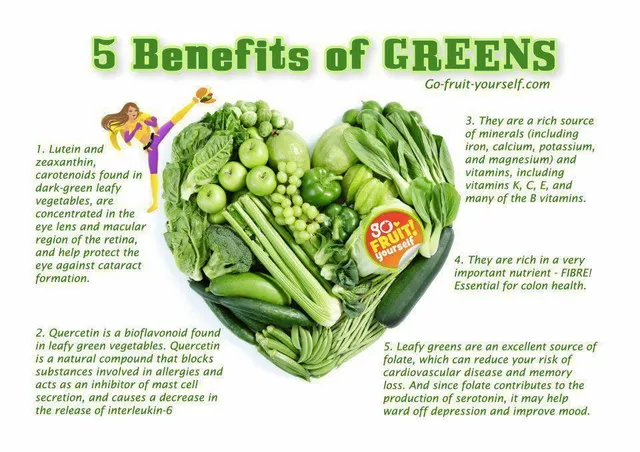
Folate Deficiency and Eye Health: What You Need to Know
As a blogger, I recently came across an important topic concerning eye health - folate deficiency. Folate, also known as vitamin B9, plays a crucial role in maintaining our overall well-being, including our precious eyesight. A deficiency in folate can lead to various eye problems, such as macular degeneration and optic neuropathy. To prevent these issues, it's essential to consume a balanced diet rich in leafy greens, beans, and fortified cereals. So, let's take care of our eyes by ensuring we get enough folate in our daily diets!
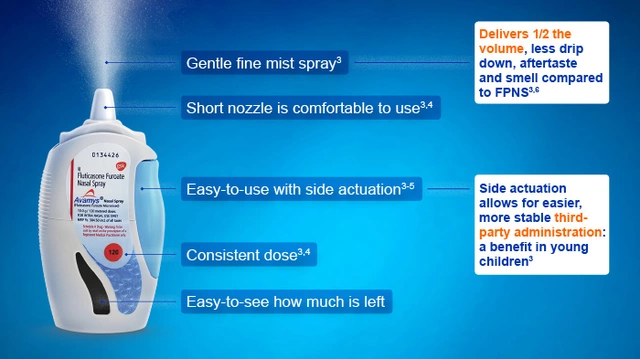
Fluticasone for Travelers: Managing Allergies on the Go
As a traveler, I've found that fluticasone is a game changer in managing allergies on the go. This nasal spray helps reduce inflammation and control common allergy symptoms, allowing me to fully enjoy my trips without constantly sneezing or dealing with itchy eyes. It's easy to pack and use, making it a must-have in my travel essentials. I highly recommend fluticasone for fellow travelers who suffer from allergies, as it makes exploring new places so much more enjoyable. Remember to consult with your doctor before using any medication, especially if you're planning an adventure abroad!
Priscilla Kraft
January 10, 2026 AT 13:50Just had my mom get hospitalized last year from a silent NSAID bleed-she’d been taking naproxen daily for 5 years thinking it was ‘just pain relief.’ No warning, no pain, just extreme fatigue. She’s on omeprazole now and feels like a new person. If you’re over 60 and on NSAIDs, please, please talk to your doctor. It’s not scare tactics-it’s survival. 🙏❤️