
Health systems aren’t waiting for the next crisis. With healthcare workforce shortage hitting record levels, hospitals and clinics across the U.S. and beyond are running on emergency mode - but not just by hiring more bodies. They’re rebuilding how work gets done, who does it, and what tools support them. The numbers don’t lie: by 2026, the U.S. could be short 3.2 million healthcare workers. Nurses, techs, doctors, and even administrative staff are stretched thin. Burnout is at 63%, and nearly half of nurses are thinking about quitting. So what’s actually working?
Stretching what you have: cross-training and flexible scheduling
Instead of just adding more staff, many hospitals are making better use of who’s already there. Cross-training has become a standard tactic - nurses learning basic phlebotomy, medical assistants handling intake forms, and even administrative staff managing simple billing tasks. Forty-three percent of hospitals now use this approach, according to the American Nurses Association. It reduces bottlenecks and gives employees more variety in their day - which helps with morale.
Flexible scheduling is another quiet game-changer. Shifts aren’t one-size-fits-all anymore. Some nurses work three 12-hour shifts. Others do four 10-hour days. Some get weekends off in exchange for weekday nights. Thirty-seven percent of major hospital systems ran pilot programs with flexible schedules, and burnout dropped by 19%. At Cleveland Clinic, flexible shifts cut turnover by 25%. It’s not just about rest - it’s about control. When people can choose when they work, they’re less likely to leave.
Bringing in outside help - but smarter
Travel nurses were once seen as a last resort. Now, they’re part of the regular plan. Twelve point seven percent of U.S. hospitals used travel nurses during peak times in 2023. But the real shift is in how they’re managed. Instead of relying on dozens of agencies, big systems like Kaiser Permanente are building their own internal staffing models. That cuts agency fees and gives them more control over quality and fit. They’ve reduced external agency reliance by 28%.
Per diem staff - those hired day-by-day - are also growing. Twenty-two percent of facilities now use them, especially for holidays, flu season, or sudden surges. International hires are up too. Eighteen percent of U.S. hospitals are recruiting globally, especially for nurses and radiology techs. It’s not a perfect fix - visa delays and cultural adaptation take time - but it’s filling critical gaps.
AI isn’t replacing people - it’s unburdening them
Artificial intelligence isn’t here to take jobs away. It’s here to take the boring stuff off people’s plates. At Baptist Health, with 23,000 employees, AI-powered document processing cut administrative work by 37%. That means nurses aren’t spending hours entering data into systems. They’re spending it with patients.
Generative AI spending in healthcare is expected to jump 51% from 2024 to 2025. Tools now auto-summarize patient notes, suggest discharge plans, flag medication errors, and even schedule follow-ups. IDC predicts the industry will save $382 billion by 2027 just by automating routine tasks. That’s not sci-fi - it’s happening now in hospitals from Atlanta to Seattle.

Keeping people from leaving: money, support, and growth
Signing bonuses? They’re common now. Most hospitals offer $15,000 to $25,000 just to walk in the door. Tuition reimbursement is offered by 68% of major systems. Loan forgiveness programs are used by 57% of public hospitals. These aren’t perks - they’re survival tools.
But money alone doesn’t keep people. Mental health support is becoming standard. Hospitals are hiring dedicated wellness coordinators, offering free counseling, and running peer support groups. One study found mental health programs reduced turnover by 17%.
And career paths? Big factor. Nurses don’t just want to stay - they want to grow. Accelerated nursing programs have nearly doubled graduate numbers since 2013. Micro-credentials - short certifications in areas like wound care or diabetes management - are now used by 29% of systems. They give staff a sense of progress without going back to school for years. Retention jumped 23% where these programs exist.
Changing where care happens
Not every patient needs to be in a hospital. That’s the new mantra. Team-based care - where nurse practitioners and physician assistants handle routine visits while doctors focus on complex cases - is now used by 78% of primary care clinics. Patient capacity went up 33% without adding more doctors.
Home-based care is expanding fast. CMS reported a 22% drop in hospital readmissions thanks to better in-home monitoring and support. For older adults and people with chronic conditions, this isn’t just convenient - it’s life-changing. It also frees up hospital beds for emergencies.

Building the next generation - from the ground up
Long-term fixes need to start early. Mayo Clinic partnered with local community colleges in Minnesota to create a pipeline for rural healthcare workers. Between 2022 and 2024, their local hire rate jumped 47%. Johns Hopkins introduced phased retirement for nursing faculty - letting them teach part-time with full benefits. Retention rose 22%.
States are joining in. The National Governors Association launched a Learning Collaborative that helped 34 states build partnerships between hospitals and local schools. These aren’t just internships - they’re guaranteed job pathways. Students get paid while learning. Hospitals get trained workers. It’s a win.
The gap still exists - and it’s growing
But let’s be clear: none of this is a magic bullet. Sixty-three percent of healthcare workers still report burnout. Forty-two percent of nurses say they’re considering quitting. And in low-income countries, 83% of facilities don’t even have basic workforce planning tools. The U.S. has resources. Many others don’t.
What’s working best? Systems that combine tactics. Intermountain Healthcare slashed vacancy rates from 18% to 7% in two years by doing three things at once: flexible scheduling, AI tools, and community college partnerships. Cleveland Clinic boosted retention by 34% with career pathways, AI training, and flexible shifts.
The message? You can’t fix a broken system with one fix. You need layers - immediate relief, smart tech, better support, and long-term investment in people. The systems that survive aren’t the ones with the biggest budgets. They’re the ones that listen to their staff - and act.
What’s next?
Eighty-nine percent of healthcare leaders plan to spend more on AI and automation by 2026. That’s not hype - it’s necessity. But the real winners will be those who use tech to empower, not replace. Nurses who spend more time with patients. Techs who aren’t buried in paperwork. Administrators who can focus on strategy instead of scheduling.
The future of healthcare isn’t about having more people. It’s about making the people you have more effective, more supported, and more valued. That’s the real shortage we’re solving.
15 Comments
Write a comment
More Articles

Prepaid Drug Mail-Back Envelopes for Medication Disposal: How They Work and Where to Get Them
Prepaid drug mail-back envelopes let you safely dispose of expired or unused medications by mail-no trips to a pharmacy needed. Learn how they work, what you can send, and where to get them for free.
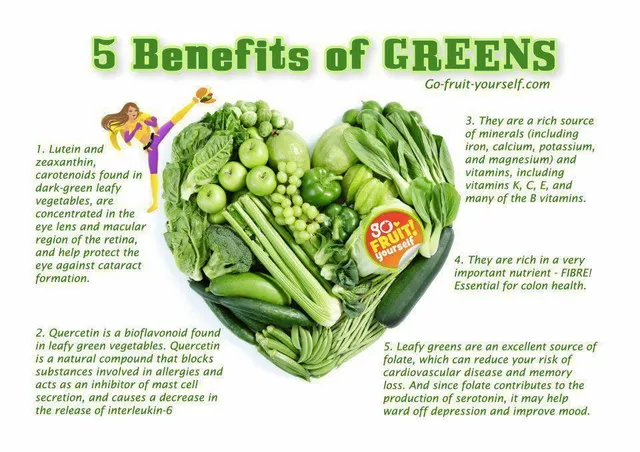
Folate Deficiency and Eye Health: What You Need to Know
As a blogger, I recently came across an important topic concerning eye health - folate deficiency. Folate, also known as vitamin B9, plays a crucial role in maintaining our overall well-being, including our precious eyesight. A deficiency in folate can lead to various eye problems, such as macular degeneration and optic neuropathy. To prevent these issues, it's essential to consume a balanced diet rich in leafy greens, beans, and fortified cereals. So, let's take care of our eyes by ensuring we get enough folate in our daily diets!
zac grant
December 3, 2025 AT 17:08AI is the real MVP here. At my hospital, we cut documentation time by almost 40% with automated note summarization. Nurses are actually smiling again. Not because they’re working less, but because they’re doing what they trained for - caring for patients, not chasing keystrokes.