
If you’ve ever woken up with a burning chest or a sour taste in your mouth, you’re not alone. About 7% of adults in the U.S. have daily acid reflux symptoms - and many of them are taking proton pump inhibitors (PPIs) to manage it. But here’s the catch: PPIs aren’t a cure. They’re a tool. And the real key to long-term relief? Lifestyle changes that actually stick.
What’s Really Going On With GERD?
GERD isn’t just occasional heartburn. It’s when the muscle at the bottom of your esophagus - called the lower esophageal sphincter (LES) - stops working right. Instead of staying shut after food goes in, it lets stomach acid sneak back up. That acid burns the lining of your esophagus, which isn’t built to handle it. The result? Pain, regurgitation, chronic cough, hoarseness, even bad breath. This isn’t new. Doctors started calling it GERD in the 1980s, after realizing some people had constant reflux, not just the occasional after-a-big-meal episode. Today, the medical definition is clear: if you have heartburn or regurgitation at least twice a week, and it’s linked to acid backing up, you’ve got GERD. The biggest risk factors? Being overweight (especially with a BMI over 30), smoking, pregnancy, and having a hiatal hernia. About 94% of people with severe esophagitis have one. Medications like calcium channel blockers for high blood pressure can also make it worse. Left untreated, GERD can lead to real problems: strictures (narrowing of the esophagus), ulcers, and Barrett’s esophagus - a condition that raises your risk of esophageal cancer. That’s why managing it isn’t just about feeling better today. It’s about protecting your body long-term.PPIs: The Strongest Acid Blockers, But Not a Forever Fix
Proton pump inhibitors - drugs like omeprazole, pantoprazole, and esomeprazole - are the go-to for GERD. They work by shutting down the acid-producing pumps in your stomach cells. That’s powerful. They reduce acid by 90-98%, and in clinical trials, they heal esophagitis in 70-90% of cases. That’s why doctors prescribe them. If you have visible damage from acid, or symptoms that won’t quit, PPIs are the fastest way to get relief. Most people take them once a day, 30-60 minutes before breakfast. That timing matters. Take them after eating, and they won’t work as well. But here’s what most people don’t know: PPIs don’t fix the broken valve. They just turn down the acid. That’s why symptoms often come back as soon as you stop. And there are risks. Long-term use - especially over a year - is linked to higher chances of:- Intestinal infections like C. diff
- Vitamin B12 deficiency
- Low magnesium levels
- Increased hip fracture risk in older adults (35% higher with 3+ years of use)
Lifestyle Changes: The Real Game-Changer
Medication helps. But lifestyle changes? They change the game. Losing just 5-10% of your body weight cuts GERD symptoms by 50%. That’s not magic. It’s physics. Extra belly fat pushes up on your stomach, forcing acid out. Even modest weight loss makes a measurable difference. Then there’s timing. Eating within two or three hours of bedtime? That’s a major trigger. Studies show cutting that out reduces nighttime acid exposure by 40-60%. Try sleeping with your head elevated 6 inches. It sounds simple, but it’s one of the most effective tricks - and it’s free. Now, the food. Not all triggers are the same for everyone. But the big ones? Coffee, tomatoes, alcohol, chocolate, fatty foods, and spicy meals. Research shows these make symptoms worse for 70-80% of people. One patient on Reddit said cutting out coffee alone gave her 70% relief. Another found eliminating spicy food cut his nighttime cough in half. The key? Track it. Use a food diary for two weeks. Write down what you eat, when you eat it, and how you feel. You’ll start seeing patterns. Maybe it’s not the pizza - it’s the soda you drink with it. Or maybe it’s the late-night snack you think is harmless. A 2022 survey found 58% of people got moderate to complete symptom control with diet and lifestyle changes alone. That’s almost 6 in 10 people who didn’t need meds to feel better.The Problem With Stopping PPIs - And How to Do It Right
Here’s the thing: when people stop PPIs cold turkey, a lot of them get worse. Not because the drug didn’t work - but because their stomach ramps up acid production in response. It’s called rebound acid hypersecretion. About 44% of users report this in studies. You can’t just quit. You have to taper. A smart approach:- Keep your PPI for now.
- Start lifestyle changes - diet, weight loss, no late meals.
- After 4-6 weeks, ask your doctor about switching to an H2 blocker like famotidine (Pepcid). These are weaker than PPIs but safer long-term.
- Use H2 blockers on an as-needed basis - only when you feel symptoms coming on.
- Slowly reduce the dose over 4-8 weeks.
When to Think Beyond Pills and Diets
Not everyone responds to meds and lifestyle. If you’ve tried everything for 8-12 weeks and still have symptoms - especially if you’re having trouble swallowing, losing weight, or seeing blood - you need an endoscopy. That’s not optional. That’s how you catch Barrett’s esophagus early. For those who still struggle, surgery is an option. Fundoplication - where the top of the stomach is wrapped around the LES - has a 90% success rate at 10 years. Newer options like the LINX® device (a small magnetic ring placed around the LES) have 85% of patients reporting symptom reduction at 5 years. And now, there’s Vonoprazan - the first new acid blocker class in 30 years. Approved in 2023, it works faster and may be more effective than PPIs for some. It’s not yet widely available, but it’s a sign that the field is evolving.
What Works Best? The Real-World Answer
The best outcome? Not PPIs alone. Not diet alone. It’s both. A 2023 Johns Hopkins study gave people a 12-week structured plan: diet, weight loss, sleep position, and stress management - no PPIs at first. After 12 weeks, 65% were able to stop PPIs completely and still feel better. The control group - just standard care - only saw a 28% success rate. That’s the difference between treating symptoms and treating the cause. PPIs are powerful. But they’re not a lifelong solution. Lifestyle changes are hard. They require planning, patience, and sometimes saying no to friends, parties, or late-night snacks. But they’re the only thing that can truly change your relationship with food - and your body. The goal isn’t to be perfect. It’s to be consistent. Skip the coffee one morning. Eat dinner at 7 instead of 9. Walk after eating. Elevate your bed. These aren’t just tips. They’re tools. And together, they can do what no pill can: give you back your life without depending on medication.What to Do Next
If you’re on PPIs right now:- Ask your doctor: “Is this still necessary?”
- Start a food and symptom diary for two weeks.
- Try cutting out the top 3 triggers: coffee, alcohol, and late meals.
- Don’t stop your PPI suddenly. Work with your provider to taper safely.
- If symptoms persist after 8 weeks of lifestyle changes, ask about an endoscopy.
- Don’t wait until it’s “bad enough.”
- Start with weight loss - even 5% helps.
- Give yourself 4-6 weeks to adjust. Symptoms don’t vanish overnight.
- Use apps like RefluxMD to track triggers - they’re rated 4.7/5 by thousands.
Can I stop taking PPIs on my own?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, making your symptoms worse for days or weeks. Always work with your doctor to taper off slowly - often by switching to an H2 blocker like famotidine first, then reducing gradually over 4-8 weeks.
Do I need to avoid all trigger foods forever?
Not necessarily. Everyone’s triggers are different. Some people can have a small amount of chocolate or wine without issues. The key is to test foods one at a time after symptoms improve. Keep a food diary to find your personal triggers - not just the common ones. Once you know what affects you, you can plan around it instead of avoiding everything.
Is GERD the same as heartburn?
Heartburn is a symptom. GERD is the chronic condition that causes frequent heartburn - at least twice a week - along with other signs like regurgitation, chronic cough, or hoarseness. Occasional heartburn after a big meal is normal. If it’s happening regularly, it’s likely GERD.
Can lifestyle changes really heal esophagitis?
Yes - but not always alone. For mild cases, diet, weight loss, and avoiding late meals can reduce inflammation enough for the esophagus to heal. For moderate to severe cases, PPIs are still needed to speed healing. But lifestyle changes are what keep it healed long-term. Studies show people who combine both have the lowest relapse rates.
Why do I still feel symptoms even though my PPI is working?
PPIs reduce acid, but they don’t fix the physical leak. If you’re still getting symptoms, it could be because you’re still eating trigger foods, lying down too soon after meals, or not taking the PPI correctly (it needs to be taken before food). Also, some symptoms like cough or hoarseness may be caused by acid reaching your throat - which PPIs don’t always stop completely. Lifestyle changes help block that path.
Is surgery worth considering for GERD?
Surgery is usually an option if you’ve tried 8-12 weeks of lifestyle changes and medication and still have severe symptoms, or if you can’t tolerate long-term PPI use. Procedures like fundoplication or LINX® have high success rates - 85-90% - and many patients report better quality of life than with daily pills. But surgery isn’t risk-free. Talk to a specialist to see if you’re a candidate.
12 Comments
Write a comment
More Articles

Unlock Your Body's Full Potential with Androstenetrione: The Groundbreaking Dietary Supplement
Discover the power of Androstenetrione, a revolutionary dietary supplement designed to unlock your body's full potential. This game-changing supplement works by naturally boosting your hormone levels, meaning you can achieve your fitness goals more easily. You'll notice improvements in your strength, endurance, and overall performance. It's not just for athletes though - anyone can benefit from the increased energy and vitality that Androstenetrione brings. Trust me, it's a total game-changer.
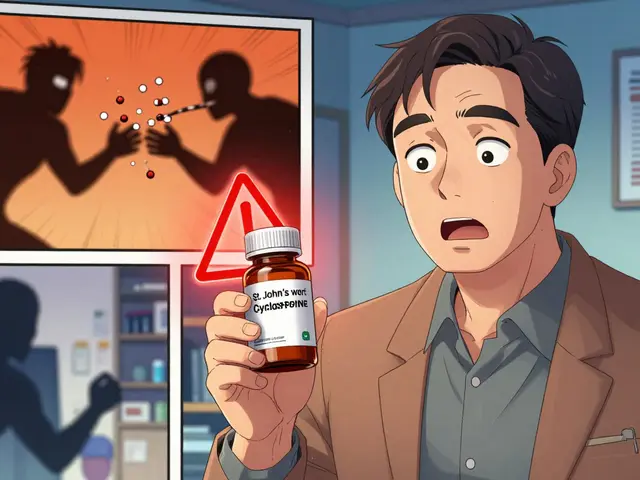
Dietary Supplement-Drug Interactions: What You Need to Know for Safety
Dietary supplement-drug interactions can cause serious health risks, from bleeding to organ rejection. Learn which supplements clash with common medications and how to protect yourself.

Traveling with Parkinsonism: Tips for a Successful Trip
Traveling with Parkinsonism can be challenging, but with proper planning and preparation, it is definitely possible to have a successful trip. In my latest blog post, I share some essential tips for making your journey as smooth and enjoyable as possible. Some key suggestions include discussing travel plans with your healthcare team, making necessary medication adjustments, and researching accessibility and support services at your destination. I also emphasize the importance of packing smart and staying flexible during the trip. Give it a read to ensure a memorable and stress-free vacation despite Parkinsonism!
Darren McGuff
January 9, 2026 AT 18:47Let me tell you something most doctors won’t: PPIs are the opioid of GI medicine. We’ve been overprescribing them like candy while ignoring the root cause. I’ve seen patients go from ‘I can’t sleep’ to ‘I feel like a new person’ after ditching the pill and just cutting out midnight snacks and losing 8% of their body weight. No magic, just physics and discipline.