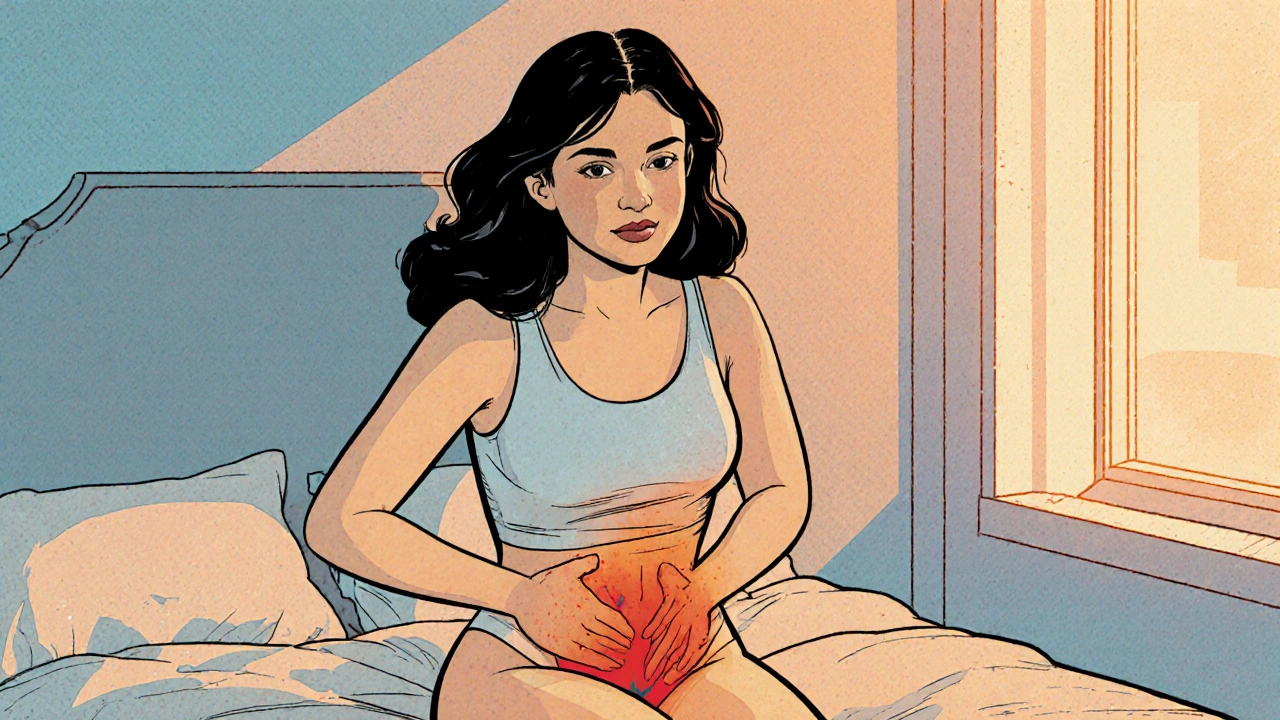
Chronic Pelvic Pain: Understanding, Diagnosing, and Treating the Condition
When dealing with chronic pelvic pain, persistent discomfort in the lower abdomen or pelvis lasting more than six months. Also known as CPP, it often signals deeper issues that need careful evaluation. You’ll notice that chronic pelvic pain isn’t a single disease; it’s a symptom umbrella that pulls in gynecologic, urologic, gastrointestinal, and musculoskeletal factors. One of the biggest contributors is endometriosis, tissue similar to the uterine lining growing outside the uterus, which can cause scar tissue, adhesions, and relentless aching. Another key player is pelvic floor dysfunction, weakness or spasm of the muscles that support the pelvic organs. These two entities together explain why many patients report pain that intensifies during periods, intercourse, or prolonged sitting.
How clinicians assess and treat the pain
Diagnosing chronic pelvic pain starts with a detailed history and a focused physical exam; clinicians look for red‑flag signs that point to infection or cancer. Imaging such as pelvic MRI or ultrasound helps rule out structural problems, while pain questionnaires capture the neuropathic component. When neuropathic pain is part of the picture, medications like gabapentin or low‑dose tricyclic antidepressants become useful tools. Physical therapy that targets the pelvic floor can restore muscle balance, and minimally invasive surgery may be an option for severe endometriosis. Lifestyle tweaks—regular low‑impact exercise, stress‑reduction techniques, and dietary tweaks—also play a role in easing the discomfort.
Because chronic pelvic pain often overlaps with conditions such as interstitial cystitis, irritable bowel syndrome, or pudendal neuralgia, an interdisciplinary approach works best. Urologists, gynecologists, gastroenterologists, pain specialists, and physical therapists team up to create a personalized plan. The goal isn’t just to mask the pain but to address the underlying mechanisms, improve daily function, and prevent flare‑ups. Below you’ll find a curated set of articles that dive deeper into medication choices, therapeutic techniques, and real‑world coping strategies for anyone navigating this complex symptom.
Understanding Vaginal Burning and Its Connection to Chronic Pelvic Pain
Explore how vaginal burning can signal chronic pelvic pain, its causes, diagnosis, and practical treatment steps for lasting relief.