Glaucoma treatment: Practical options to protect your vision
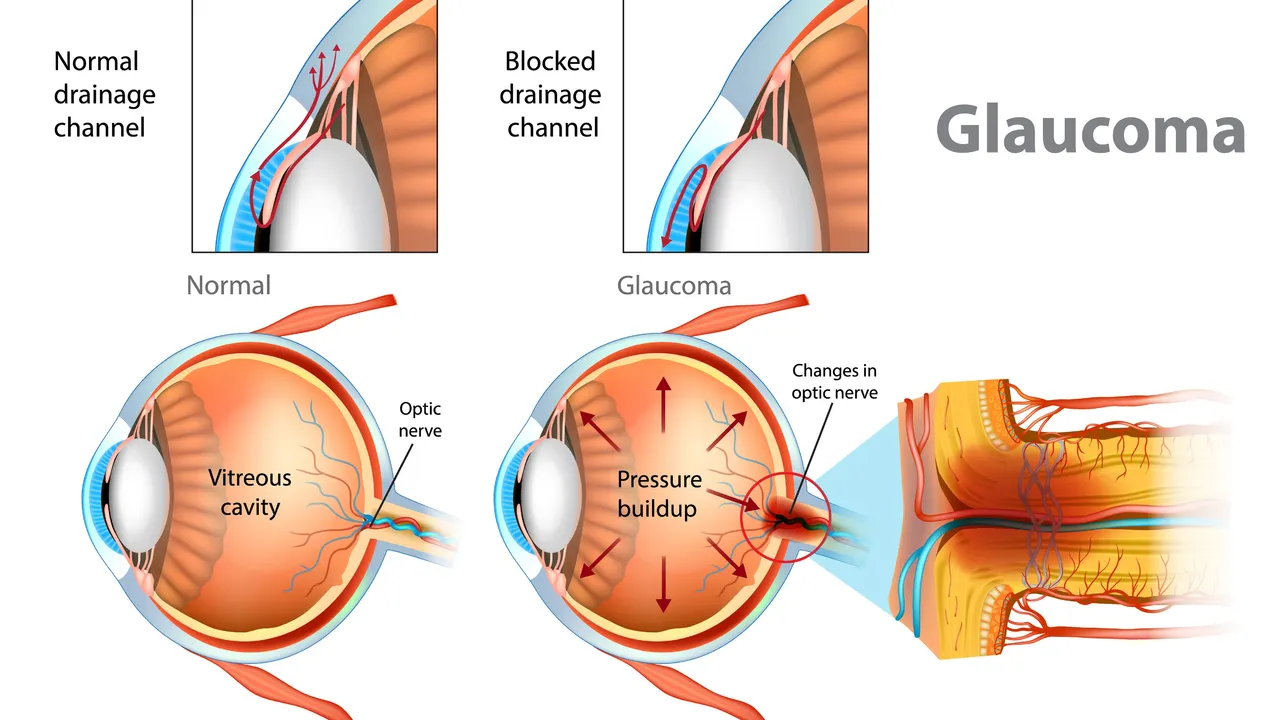
Glaucoma is a leading cause of blindness worldwide — but early treatment can slow or stop vision loss. Want straight answers about what helps? Below I explain common choices, when doctors use them, and what you should watch for.
Eye drops are the most common first step. Prostaglandin analogs (like latanoprost) lower pressure overnight and often work well with once-a-day dosing. Beta-blockers (timolol) reduce fluid production, and carbonic anhydrase inhibitors or alpha agonists lower pressure in different ways. Many people use combination drops to cut the number of bottles. Side effects range from mild irritation and eye color change with prostaglandins to breathing or heart effects with beta-blockers, so tell your doctor about asthma or heart problems. Missing doses is the biggest reason treatment fails — set a routine or use phone reminders.
If drops aren't enough or cause problems, laser treatment is a clear next option. Selective laser trabeculoplasty (SLT) is common for open-angle glaucoma. It lowers pressure by helping drainage and can delay or reduce the need for drops. SLT is quick, done in clinic, and recovery is short, though some people need repeat treatment. For angle-closure glaucoma, a laser iridotomy creates a small hole in the iris to unblock fluid flow — this can be urgent.
Surgery is for cases where drops and laser don't control pressure. Trabeculectomy creates a new drainage path and usually lowers pressure a lot, but it requires close follow-up because of infection or scarring risks. Tube shunt implants are another option, especially after failed surgeries. In recent years, MIGS (minimally invasive glaucoma surgery) has become popular for mild to moderate disease; MIGS has a faster recovery but often achieves more modest pressure drops.
Monitoring matters. Regular eye pressure checks, visual field tests, and optic nerve imaging (OCT) tell your care team if damage is progressing. Your target pressure should be personalized — older adults with slow damage may tolerate higher pressures than younger people with fast loss. Keep a log of symptoms and medication side effects so you and your doctor can spot changes quickly.
Small lifestyle steps help but don't replace medical care. Exercise, staying hydrated without big fluid spikes, and avoiding medications that raise eye pressure (ask your pharmacist about over-the-counter cold medicines) can support treatment. If you have sudden eye pain, redness, nausea, or rapid vision changes, get emergency care — angle-closure glaucoma can be an emergency.
Ask your eye doctor practical questions: What pressure target do you aim for? How will we measure progress? What side effects should I report? When might I need laser or surgery? If a second opinion would make you feel better, ask for one. Glaucoma management is a long-term partnership — the right plan protects what you can still see.
Family history matters — first-degree relatives should get regular checks. Talk about cost and generic eye drops; many are cheaper and work the same. Use drop guides or ask a nurse to show technique. Small changes make big differences over years daily.
The effectiveness of dorzolamide in treating different types of glaucoma
Hey there, gentlemen! I just wanted to share some insights on a very interesting topic - the effectiveness of dorzolamide in treating different types of glaucoma. We'll dive into its mechanism of action, its beneficial effects on different types of this eye condition, and why it's becoming a go-to medication. Through this, I hope to provide everyone with a deeper understanding of this treatment option in a clear and simple language. Remember, knowledge is your best ally in health matters!