Key Takeaways
- Brimonidine tartrate is an alpha‑2 adrenergic agonist that both cuts fluid production and boosts outflow.
- Prostaglandin analogs (latanoprost, travoprost, bimatoprost) usually give the biggest pressure drop but may cause iris darkening.
- Beta‑blockers like timolol work well for people who can’t tolerate prostaglandins but are off‑limits if you have asthma or certain heart issues.
- Carbonic anhydrase inhibitors (dorzolamide, brinzolamide) are useful as add‑on drops when a single drug isn’t enough.
- Choosing the right eye drop depends on efficacy, side‑effect profile, dosing convenience, and any systemic health concerns you have.
When treating open‑angle glaucoma, Brimonidine tartrate is a selective alpha‑2 adrenergic agonist that lowers intra‑ocular pressure by reducing aqueous humor production and increasing uveoscleral outflow. It’s been on the market for over two decades, yet many patients still wonder how it stacks up against the newer prostaglandin analogs or the classic beta‑blocker timolol. This guide compares brimonidine with the most commonly prescribed glaucoma drops, walks through the science behind each class, and offers practical questions to ask your ophthalmologist.
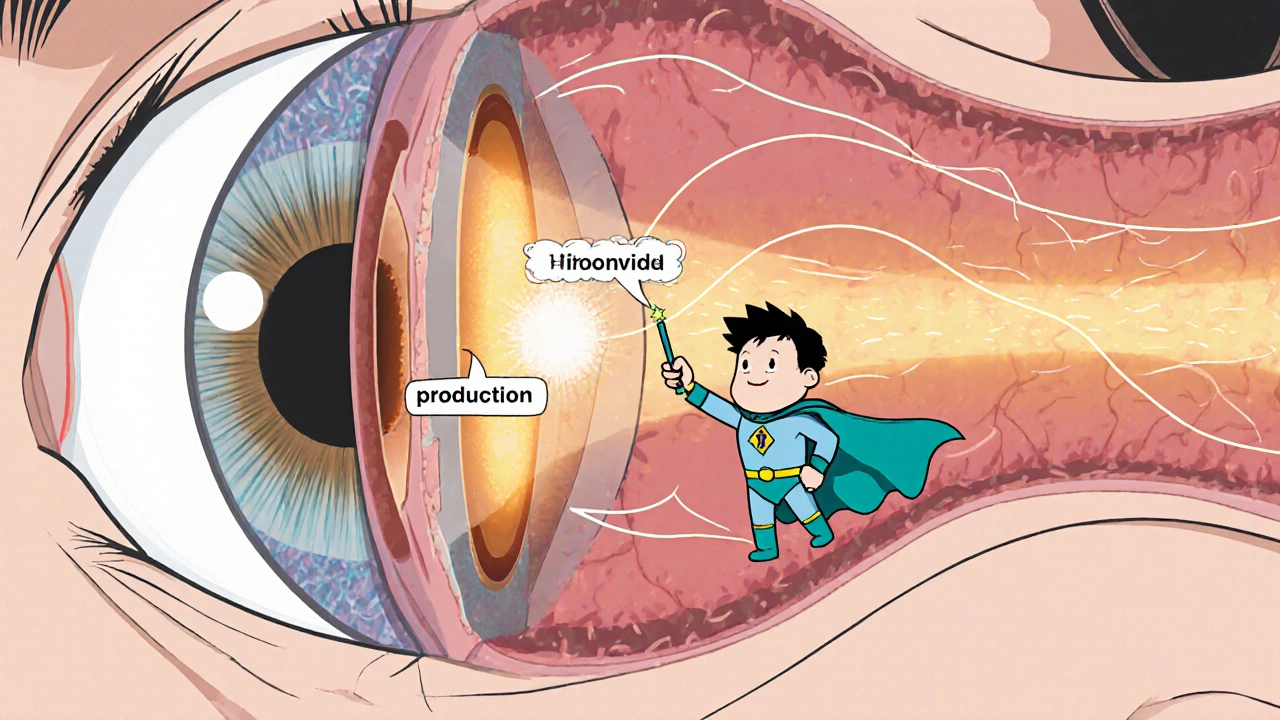
How Brimonidine Works
Brimonidine binds to alpha‑2 receptors in the ciliary body. This binding does two things: it tells the eye to make less aqueous humor, and it nudges the drainage pathways to let more fluid escape. The net result is a 20‑30 % drop in intra‑ocular pressure (IOP) after twice‑daily dosing.
Because it hits two mechanisms, brimonidine can be a solid stand‑alone therapy, especially for patients who need a non‑prostaglandin option. However, the drug can cause ocular redness, allergic‑type reactions, and a dry‑eye feel. Systemically, it may lower blood pressure a bit, so doctors keep an eye on patients with a history of hypotension.
Major Classes of Glaucoma Medications
Below are the drug families you’ll most likely encounter. Each class has a distinctive mechanism, dosing schedule, and side‑effect fingerprint.
- Prostaglandin analogs (e.g., latanoprost, travoprost, bimatoprost) - increase uveoscleral outflow; usually once‑daily at night.
- Beta‑blockers (e.g., timolol) - reduce aqueous production; often twice‑daily.
- Carbonic anhydrase inhibitors (e.g., dorzolamide, brinzolamide) - block fluid‑producing enzyme; typically twice‑daily.
- Alpha‑2 adrenergic agonists (brimonidine tartrate) - dual action on production and outflow; twice‑daily.
- Cholinergic agents (e.g., pilocarpine) - enhance trabecular outflow; multiple doses per day.
Side‑Effect Snapshot
| Class | Typical side effects | Systemic concerns |
|---|---|---|
| Prostaglandin analogs | Eye redness, eyelash growth, iris darkening | Rarely systemic; generally safe |
| Beta‑blockers | Burning, dry eye, reduced tear production | Bradycardia, asthma exacerbation, COPD |
| Carbonic anhydrase inhibitors | Metallic taste, bitter mouth, ocular discomfort | Electrolyte imbalances, kidney stones (rare) |
| Alpha‑2 agonists | Redness, allergic‑type reaction, fatigue | Low blood pressure, dry mouth |
| Cholinergic agents | Blurred vision, brow ache, iris constriction | Systemic cholinergic effects (rare) |
Direct Comparison: Efficacy and Convenience
| Medication | Mechanism | Typical dosing | Average IOP reduction | Notable side effects |
|---|---|---|---|---|
| Brimonidine tartrate | Alpha‑2 agonist | Twice daily | 20‑30 % | Redness, fatigue, possible hypotension |
| Latanoprost | Prostaglandin analog | Once nightly | 25‑35 % | Eyebrow growth, iris darkening, mild redness |
| Timolol | Beta‑blocker | Twice daily | 20‑25 % | Bradycardia, bronchospasm, dry eye |
| Dorzolamide | Carbonic anhydrase inhibitor | Twice daily | 15‑20 % | Metallic taste, rare kidney issues |
| Pilocarpine | Cholinergic agent | Three‑four times daily | 10‑15 % | Blurred vision, brow ache |
Numbers come from large‑scale clinical trials and meta‑analyses up to 2024. The biggest takeaway: prostaglandin analogs still lead in pressure‑lowering power, but brimonidine holds its own and offers a twice‑daily schedule that some patients find easier than three‑ or four‑times‑daily drops.
Factors to Consider When Picking a Drop
- How much pressure needs to drop? If your baseline IOP is >30 mmHg, a prostaglandin analog is often first‑line.
- Any respiratory or cardiac conditions? Avoid beta‑blockers if you have asthma, COPD, or heart block.
- Do you have dry‑eye or allergic tendencies? Brimonidine’s redness can be a deal‑breaker; prostaglandins may worsen ocular surface disease for some.
- Convenience matters. Once‑daily night dosing fits busy schedules, whereas twice‑daily might be easier for people who already have a morning‑evening routine.
- Cost and insurance coverage. Generic timolol and dorzolamide are cheap; branded prostaglandins can be pricey without formulary support.
Write down your answers before the appointment. A clear picture helps the ophthalmologist tailor the regimen.
Practical Tips for Using Eye Drops Effectively
- Wash hands, avoid touching the tip, and tilt your head back.
- Pull down the lower eyelid to create a small pocket, squeeze the prescribed number of drops, then close the eye gently for 1‑2 minutes.
- If you need two different drops, wait at least five minutes between them to prevent wash‑out.
- Keep a diary for the first two weeks; note any redness, stinging, or visual changes and report them.
When Brimonidine Might Be the Best Choice
Patients who can’t tolerate prostaglandin‑induced iris changes, who have contraindications to beta‑blockers, or who need a drug that also offers mild neuroprotective effects may find brimonidine ideal. Some studies suggest it may help preserve retinal ganglion cells beyond pressure control, though the evidence is still emerging.
Potential Pitfalls and How to Avoid Them
Because brimonidine lowers systemic blood pressure, people on antihypertensives should have their vitals checked after starting therapy. Also, the “red eye” reaction can mimic infection; if redness persists beyond a week or is accompanied by discharge, seek medical advice.
Frequently Asked Questions
Can I use brimonidine with other eye drops?
Yes. Most doctors prescribe brimonidine as part of a combination regimen, especially if a single drug isn’t enough. Just space drops by five minutes.
How long does it take to see a pressure drop?
You’ll usually notice a reduction within 2‑4 weeks of consistent use. Follow‑up tonometry is essential to confirm the effect.
Is brimonidine safe for children?
It’s approved for pediatric use in certain types of glaucoma, but dosing is weight‑based. A pediatric ophthalmologist should manage it.
What should I do if I miss a dose?
Take the missed drop as soon as you remember unless it’s close to the next scheduled dose. In that case, skip the missed one and continue with your regular schedule.
Are there generic versions of brimonidine?
Yes. Generic brimonidine tartrate is available in many markets and is usually covered by insurance plans.
Choosing the right glaucoma medication isn’t a one‑size‑fits‑all decision. By understanding how brimonidine compares to prostaglandin analogs, beta‑blockers, carbonic anhydrase inhibitors, and cholinergic agents, you can have an informed conversation with your eye doctor and land on a regimen that balances efficacy, comfort, and your overall health.
9 Comments
Write a comment
More Articles

Buy Cheap Generic Zyrtec Online - Safe Guide & Best Prices 2025
Learn how to safely buy cheap generic Zyrtec online in the UK. Get a step‑by‑step guide, price comparison, safety tips, and a checklist to avoid scams.
Palliative and Hospice Care: How to Balance Symptom Relief with Minimal Side Effects
Learn how palliative and hospice care balance pain relief with minimal side effects. Discover practical strategies for managing symptoms like breathlessness, delirium, and nausea while preserving dignity and quality of life.

Rakhi Kasana
October 18, 2025 AT 22:48Brimonidine is an underrated option if you hate prostaglandin‑induced iris darkening.