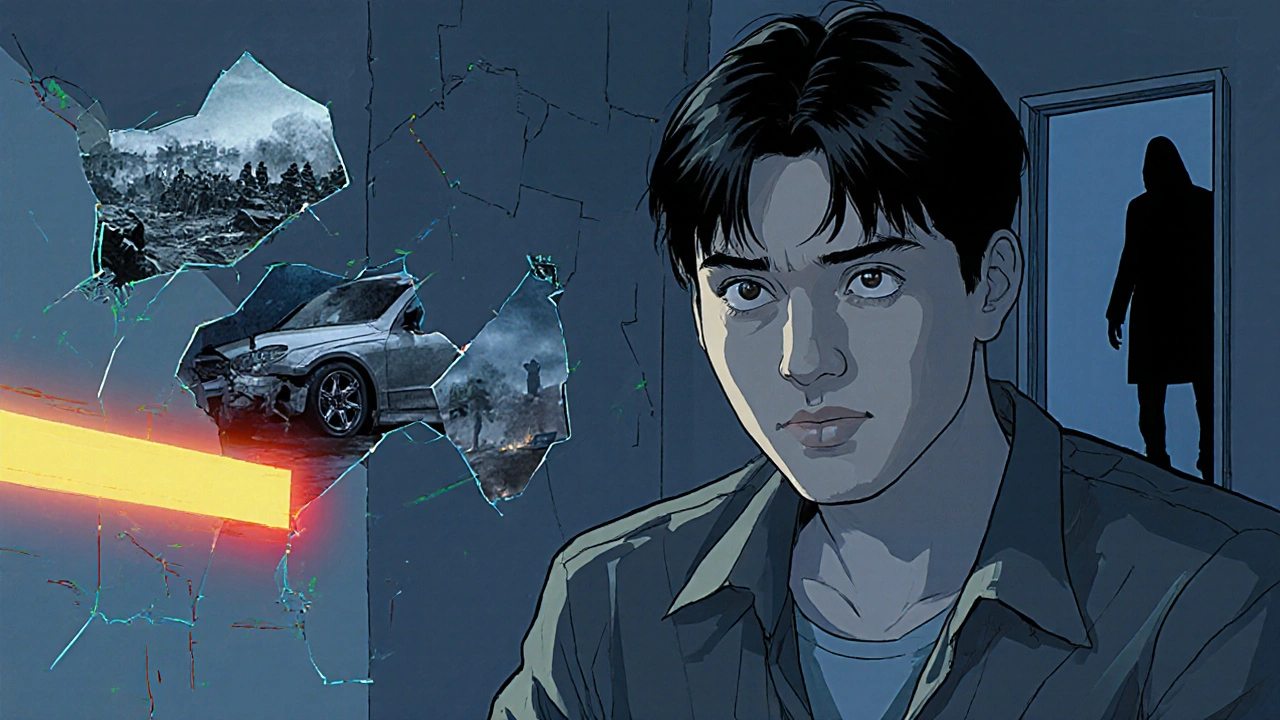
Posttraumatic Stress Disorder – Overview and Resources
When dealing with posttraumatic stress disorder, a mental health condition triggered by intense or life‑threatening events. Also known as PTSD, it can disrupt sleep, memory, and relationships. posttraumatic stress disorder typically shows up after a person experiences trauma, the severe psychological impact of witnessing or enduring a threat to one's safety. The condition brings together three core clusters: intrusive memories that replay the event, heightened arousal that keeps the nervous system on edge, and avoidance behaviors that limit everyday activities. These symptoms don’t appear in a vacuum; they often intersect with depression, a persistent low mood that can worsen stress‑related outcomes and amplify functional impairment. Because PTSD touches the brain’s fear‑processing circuits, it frequently co‑exists with anxiety disorders, making diagnosis and treatment more complex. Understanding the relationship between trauma exposure, anxiety, and depression is essential for choosing the right therapeutic path.
Key Concepts and Co‑occurring Conditions
Effective management of posttraumatic stress disorder rests on two pillars: evidence‑based psychotherapy and, when appropriate, medication. Cognitive Behavioral Therapy (CBT), especially trauma‑focused variants like Prolonged Exposure and Cognitive Processing Therapy, directly targets the intrusive memories and maladaptive beliefs that keep the fear cycle alive. These approaches require patients to confront avoided memories in a safe environment, reshaping the brain’s response to trauma cues. Alongside CBT, selective serotonin reuptake inhibitors (SSRIs) such as sertraline and paroxetine can reduce both PTSD and overlapping depressive symptoms, stabilizing mood and improving sleep. The Naranjo Scale, a tool for assessing drug reaction causality, sometimes helps clinicians decide if side effects are medication‑related or part of the disorder’s symptom load. In practice, clinicians weigh factors like symptom severity, comorbid depression, and patient preference before combining therapy with medication. Real‑world case studies show that patients who receive both CBT and an SSRI often experience faster symptom relief than those who rely on a single modality.
Beyond formal treatment, everyday strategies can buffer the impact of PTSD. Regular physical activity helps regulate stress hormones, while mindfulness practices lower baseline arousal and improve emotional regulation. Social support—whether from family, support groups, or peer mentors—acts as a protective factor against isolation, which can deepen depressive episodes. When you’re ready to dive deeper, the articles below break down specific topics: how paroxetine helps with related mood disorders, practical tips for supporting a partner with depressive disorder, and guidance on assessing medication side effects. Together they form a toolkit you can use to understand, manage, and eventually move beyond posttraumatic stress disorder.
Art Therapy for PTSD: How It Helps and What to Expect
Discover how art therapy reduces PTSD symptoms, the science behind it, practical steps, and tips for finding the right program.