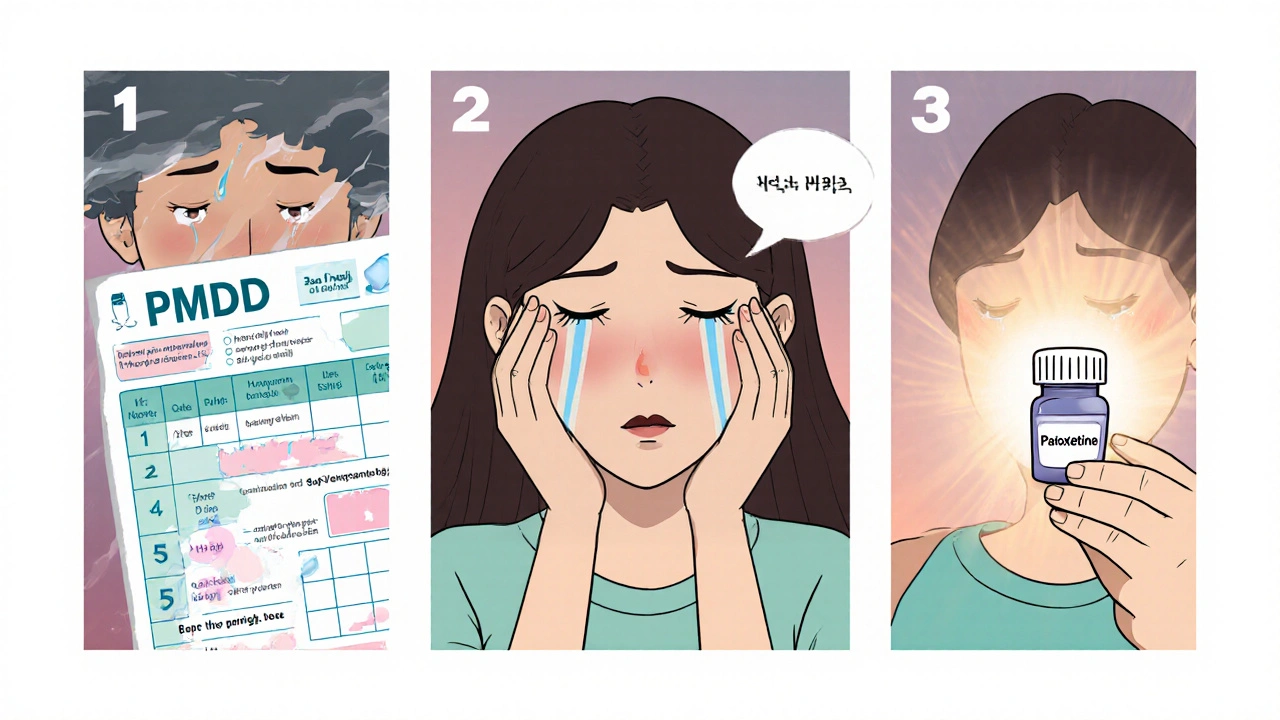
PMDD Treatment Timeline Calculator
Enter when you begin paroxetine treatment to see when symptom relief may start.
Key Takeaways
- Paroxetine is an FDA‑approved SSRI that has strong evidence for reducing PMDD symptoms.
- Typical starting dose is 10‑20mg daily, with symptom relief often appearing after 2‑3weeks.
- Common side effects (nausea, insomnia, sexual changes) are usually mild and improve over time.
- Women on other serotonergic meds or certain antidepressants should check for drug‑interaction risks.
- Paroxetine works best when combined with lifestyle tweaks like exercise, diet, and stress management.
Living with Paroxetine is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed for depression and anxiety disorders can feel like stepping into a maze of medical jargon, especially when the goal is to calm the intense mood swings of Premenstrual Dysphoric Disorder a severe form of premenstrual syndrome affecting about 5% of menstruating people, characterized by extreme irritability, depression, and physical pain. This guide cuts through the noise, explains how paroxetine works for PMDD, and gives you a realistic roadmap for starting the medication, managing side effects, and measuring success.
What Is Premenstrual Dysphoric Disorder?
Premenstrual Dysphoric Disorder is defined in the DSM‑5 as a cyclic mood disorder that occurs in the luteal phase of the menstrual cycle and resolves with the onset of menses. Unlike ordinary PMS, PMDD brings daily functioning to a halt-think severe anxiety, depressive thoughts, marked fatigue, and physical complaints like breast tenderness and bloating. Symptoms must appear at least five days before menstruation, subside shortly after bleeding begins, and be severe enough to interfere with work, school, or relationships.
Research shows that hormonal fluctuations, particularly a drop in estrogen and progesterone, interact with brain neurotransmitters, especially serotonin, to trigger the mood swings. That’s why a drug that boosts serotonin signalling-like an SSRI-has become a frontline treatment.
How Paroxetine Works
The magic behind paroxetine lies in its classification as a Selective Serotonin Reuptake Inhibitor a class of antidepressants that block the reabsorption of serotonin into neurons, increasing its availability in the synaptic cleft. By preventing serotonin from being re‑taken up, paroxetine amplifies the mood‑stabilizing effects of this neurotransmitter during the luteal phase.
Serotonin itself, serotonin a neurotransmitter that regulates mood, appetite, and sleep, plays a pivotal role in the brain’s emotional circuitry. In PMDD, the sudden hormonal dip appears to cause a brief serotonin shortage, which translates into the emotional roller‑coaster many people describe. Raising serotonin levels with paroxetine can blunt that dip, smoothing out mood swings.
The U.S. Food and Drug Administration the federal agency responsible for approving safe and effective medications approved paroxetine for PMDD in 2009, making it the first drug specifically labeled for the condition. That regulatory endorsement gives clinicians confidence that the drug’s benefits outweigh its risks when used as directed.
Clinical Evidence for Paroxetine in PMDD
Randomized, double‑blind trials have consistently shown paroxetine’s superiority over placebo for PMDD. In a landmark 2010 study involving 112 participants, women receiving 20mg of paroxetine daily reported a 55% reduction in Daily Record of Severity of Problems (DRSP) scores after three weeks, compared with a 20% drop in the placebo group. Another multi‑center trial (2015) confirmed that both immediate‑release (20mg) and delayed‑release (10mg) formulations achieved similar symptom control, with the delayed‑release version tolerating slightly fewer gastrointestinal complaints.
The drug’s rapid onset-often within two weeks-is notable because many antidepressants take six‑to‑eight weeks to show effect. This quicker response is thought to stem from the cyclical nature of PMDD; once serotonin levels are lifted during the luteal phase, the mood‑stabilizing effect persists for the remainder of the cycle.
Meta‑analyses published in 2022 aggregated data from eight trials and calculated a pooled effect size (Cohen’s d) of 0.84 for paroxetine versus placebo, classifying it as a large therapeutic impact. Importantly, the same analyses reported low dropout rates (<12%) due to adverse events, indicating that most patients tolerate the drug well enough to stay on it.
Starting Paroxetine: What to Expect
- Initial dose. Most clinicians begin with 10mg taken once daily, usually in the morning to avoid nighttime insomnia. Some start at 20mg if symptoms are severe.
- Gradual titration. If tolerability is good, the dose may be raised to 20mg after one week. The maximum recommended dose for PMDD is 40mg, but doses above 20mg rarely provide additional benefit for most patients.
- Timing with the cycle. Unlike older SSRIs that required a “pre‑treatment” phase, paroxetine can be started anytime in the month because its effect builds quickly. However, many providers advise beginning at the start of the luteal phase (around day14 of a typical 28‑day cycle) for a smoother adjustment.
- Monitoring. Symptom diaries such as the DRSP or a simple daily mood chart are essential. Look for a steady downward trend in scores after the second week of treatment.
- Duration. Most experts recommend at least three to six menstrual cycles to assess full efficacy. If significant improvement is seen, many patients stay on the medication long‑term, as stopping abruptly can trigger withdrawal or symptom rebound.
It’s worth noting that paroxetine is metabolized by the liver enzyme Cytochrome P450 2D6 a key enzyme that processes many drugs, influencing their blood levels. Genetic variations that slow CYP2D6 activity can raise paroxetine concentrations, potentially increasing side‑effect risk. If you have a known poor metabolizer status, your doctor might opt for a lower starting dose.
Managing Common Side Effects
Side effects are the most frequent reason people stop an SSRI early. With paroxetine, the top five complaints are nausea, insomnia, sexual dysfunction, headache, and increased sweating. Most are mild and fade within two weeks as the body adjusts.
- Nausea. Take the pill with food or a full glass of water. If it persists, a lower dose taken at bedtime may help.
- Insomnia. Morning dosing is key. If you still struggle to sleep, a short‑acting melatonin supplement can be used under your doctor’s guidance.
- Sexual changes. Decreased libido or delayed orgasm affect up to 30% of users. Strategies include timing sexual activity when the drug’s peak level is lowest (usually late afternoon) or discussing a “drug holiday” during the follicular phase with your clinician.
- Headache. Over‑the‑counter acetaminophen is generally safe; avoid NSAIDs if you have stomach issues.
- Sweating. Light, breathable clothing and staying hydrated can reduce discomfort.
If side effects become severe or you notice mood worsening, contact your prescriber promptly. Sometimes switching to another SSRI (e.g., sertraline) resolves the problem without sacrificing efficacy.
Paroxetine vs. Other PMPMD Treatments
| Treatment | Mechanism | Typical Onset of Relief | Common Side Effects | FDA Status for PMDD |
|---|---|---|---|---|
| Paroxetine (SSRI) | Increases synaptic serotonin | 1‑3 weeks | Nausea, insomnia, sexual changes | Approved |
| Sertraline (SSRI) | Increases synaptic serotonin | 2‑4 weeks | Diarrhea, dizziness | Off‑label |
| Oral contraceptives (estrogen‑progestin) | Stabilizes hormonal fluctuations | 1‑2 cycles | Weight gain, mood swings | Off‑label |
| Gonadotropin‑releasing hormone (GnRH) agonists | Suppresses ovarian hormone production | 1‑2 weeks | Hot flashes, bone loss | Off‑label |
| Lifestyle & CBT | Behavioral & stress‑reduction strategies | Variable (weeks‑months) | None | Not FDA‑regulated |
When you stack these options, paroxetine stands out for its rapid onset, relatively low cost, and clear regulatory backing. However, choosing the right path hinges on personal health history, tolerance for side effects, and whether you prefer a medication‑only approach or a combination with lifestyle changes.

Who Should Avoid Paroxetine?
Paroxetine isn’t safe for everyone. Absolute contraindications include:
- Current use of monoamine oxidase inhibitors (MAOIs) - a two‑week washout is mandatory.
- Known hypersensitivity to paroxetine or any of its inactive ingredients.
- Severe liver disease (since the drug is hepatically cleared).
Caution is advised for patients with:
- History of bipolar disorder - SSRI monotherapy can trigger mania.
- Pregnancy or breastfeeding - discuss risks versus benefits; SSRIs cross the placenta.
- Bleeding disorders or concurrent anticoagulant therapy - SSRIs can impair platelet aggregation.
Because paroxetine influences the placebo effect the improvement of symptoms due to a patient’s expectation rather than active drug action in clinical trials, it’s essential that the decision to start a medication be made jointly with a clinician who can monitor both therapeutic benefit and safety.
Putting It All Together: A Practical Checklist
- Confirm diagnosis of PMDD with at least two consecutive cycles using a validated symptom diary.
- Discuss medical history, especially any antidepressant use, liver issues, or bleeding risks.
- Start paroxetine at 10mg daily; increase to 20mg after one week if tolerated.
- Track daily symptoms and side effects for at least three cycles.
- Re‑evaluate with your provider after 6‑8 weeks; adjust dose or consider alternative therapy if improvement <30%.
- Maintain complementary lifestyle measures: regular exercise, omega‑3 rich diet, adequate sleep, and stress‑reduction practices.
Following this roadmap maximizes the chance that paroxetine will calm the hormonal roller‑coaster without derailing your day‑to‑day life.
Frequently Asked Questions
How long does it take for paroxetine to start working for PMDD?
Most users notice a reduction in mood symptoms within 1‑3weeks, though full cycle improvement may require 2‑3 menstrual cycles.
Can I take paroxetine only during the luteal phase?
Because the drug builds steady blood levels, many clinicians prescribe it continuously. However, some patients and doctors trial a “cycle‑limited” approach-starting a few days before symptoms begin and stopping after menstruation-to minimize exposure.
What are the most common side effects, and are they permanent?
Nausea, insomnia, and sexual changes top the list. They are usually transient, improving as your body adapts. If they persist beyond 4‑6 weeks, talk to your prescriber about dose adjustment or switching drugs.
Is paroxetine safe during pregnancy?
Evidence is mixed. SSRIs cross the placenta and have been linked to a slight increase in neonatal adaptation syndrome. Always weigh risks with your obstetrician; many clinicians switch to a non‑SSRI option before conception.
Do I need to taper off paroxetine?
Yes. Stopping abruptly can cause discontinuation syndrome (dizziness, electric‑shock sensations). A typical taper reduces the dose by 5‑10mg every 1‑2 weeks under medical supervision.
9 Comments
Write a comment
More Articles

Infographics About Generics: Visual Education Tools for Patient Understanding
Infographics about generics help patients understand why generic drugs are safe, effective, and identical to brand-name versions. Learn how visual tools are reducing confusion, lowering costs, and improving medication adherence.

The Role of Minocycline in Treating Bacterial Infections
As a blogger, I've come across some interesting information about Minocycline and its role in treating bacterial infections. This antibiotic, which belongs to the tetracycline class, has proven effective in combating a wide range of bacterial infections. Not only does Minocycline aid in treating common infections like acne and respiratory tract infections, but it also plays a crucial role in treating more severe cases, such as Lyme disease. Additionally, its anti-inflammatory properties have proven beneficial in managing certain neurological disorders. In conclusion, Minocycline is a versatile and valuable antibiotic in the fight against various bacterial infections.

Darryl Gates
October 17, 2025 AT 13:03Great overview of how paroxetine works for PMDD. The step‑by‑step guide makes it easy to follow the dosing schedule and monitor side effects. Remember to keep a symptom diary so you can see the real impact over a few cycles. Combining the medication with regular exercise and stress‑relief techniques usually yields the best results.