
Medication Food Timing Checker
Medication Food Timing Guide
Find out if your medication should be taken on an empty stomach or with food to maximize effectiveness and avoid side effects.
Have you ever taken a pill with your morning coffee, only to wonder if it even worked? You’re not alone. Millions of people take medications without thinking about what they eat-or don’t eat-around the time they swallow their pills. But the difference between taking a drug on an empty stomach or with food isn’t just a suggestion. It can mean the difference between your treatment working as it should, or failing completely.
Why Food Changes How Medicines Work
Food doesn’t just fill your stomach-it changes how your body absorbs medicine. When you eat, your stomach pH rises from super acidic (around 1-2) to much milder (3-5). That sounds small, but for some drugs, it’s enough to break them down before they even get absorbed. High-fat meals slow down how fast your stomach empties, which can delay or even block a drug from entering your bloodstream. On the flip side, food can help certain medicines dissolve better, especially ones that dissolve in fat.
Calcium in dairy, iron in spinach or supplements, and even grapefruit juice can bind to certain drugs like antibiotics, stopping them from working. A 2020 study from Pfizer showed tetracycline antibiotics lose 50-75% of their effectiveness when taken with milk or calcium-rich foods. Meanwhile, drugs like griseofulvin (used for fungal infections) absorb 50% better when taken with a fatty meal because bile released during digestion helps dissolve them.
Medications That Must Be Taken on an Empty Stomach
Some drugs are so sensitive to food that even a light snack can ruin their effect. Levothyroxine (Synthroid), used for hypothyroidism, is one of the most common offenders. A 2022 meta-analysis in the Journal of Clinical Endocrinology & Metabolism found food cuts its absorption by 20-50%. That means if you take it with breakfast, your thyroid hormone levels stay low-even if you’re taking the right dose. Patients often don’t realize their TSH levels are off because they feel fine. But over time, untreated hypothyroidism leads to fatigue, weight gain, and heart problems.
Alendronate (Fosamax), a bone-strengthening drug for osteoporosis, is another example. Merck’s 2021 prescribing info shows food reduces its absorption by 60%. That’s not just a minor drop-it means the drug won’t reach the bones where it’s needed. Taking it with coffee, orange juice, or even a glass of water that’s not plain can also interfere. The rule? Take it first thing in the morning, with a full glass of plain water, and wait at least 30 minutes before eating or drinking anything else.
Sucralfate (Carafate), used for stomach ulcers, needs to coat the ulcer lining before food arrives. If you take it after eating, the food pushes it away before it can do its job. The FDA label says take it 1 hour before meals. Same goes for ampicillin-a 2022 study showed food drops its peak concentration by 35%. Zafirlukast (Accolate), used for asthma, also loses 40% of its effect if taken with food. Even proton pump inhibitors like Nexium require you to take them at least an hour before eating, because they need to block acid production before food triggers it.
Medications That Need Food to Work Right
Not all pills hate food. Some actually need it to work safely-or at all. NSAIDs like ibuprofen and naproxen are a big one. Without food, these drugs irritate your stomach lining. A 2020 meta-analysis in Gastroenterology showed taking them with food reduces the risk of ulcers by 50-70%. Every year, 10,000 to 20,000 people in the U.S. end up in the hospital because of NSAID-related bleeding. Most of those cases could be avoided by simply eating something before popping the pill.
Aspirin, especially at higher doses for pain or inflammation, works better with food too. Bayer’s 2022 data shows stomach irritation drops from 25% to just 8% when taken with a meal. For people on daily low-dose aspirin for heart health, the risk is lower-but if you’re taking it for arthritis or headaches, food makes a real difference.
Statins like Lipitor and Zocor absorb better with food, especially meals containing fat. But here’s the catch: grapefruit juice. It doesn’t just help absorption-it overdoes it. The Canadian Medical Association Journal reported in 2023 that grapefruit juice can spike statin levels by 300-500%, raising the risk of rhabdomyolysis-a dangerous muscle breakdown that can lead to kidney failure. One glass of grapefruit juice can have this effect for over 24 hours. So even if you take your statin with food, skip the juice.
Antidepressants like duloxetine (Cymbalta) cause nausea in up to 40% of users on an empty stomach. Eli Lilly’s 2021 data shows taking it with food cuts nausea by 30%. That’s not just comfort-it’s adherence. If you’re throwing up every time you take your pill, you’ll stop taking it. And that’s when depression comes back harder.

How to Get It Right: The 2-1-2 Rule
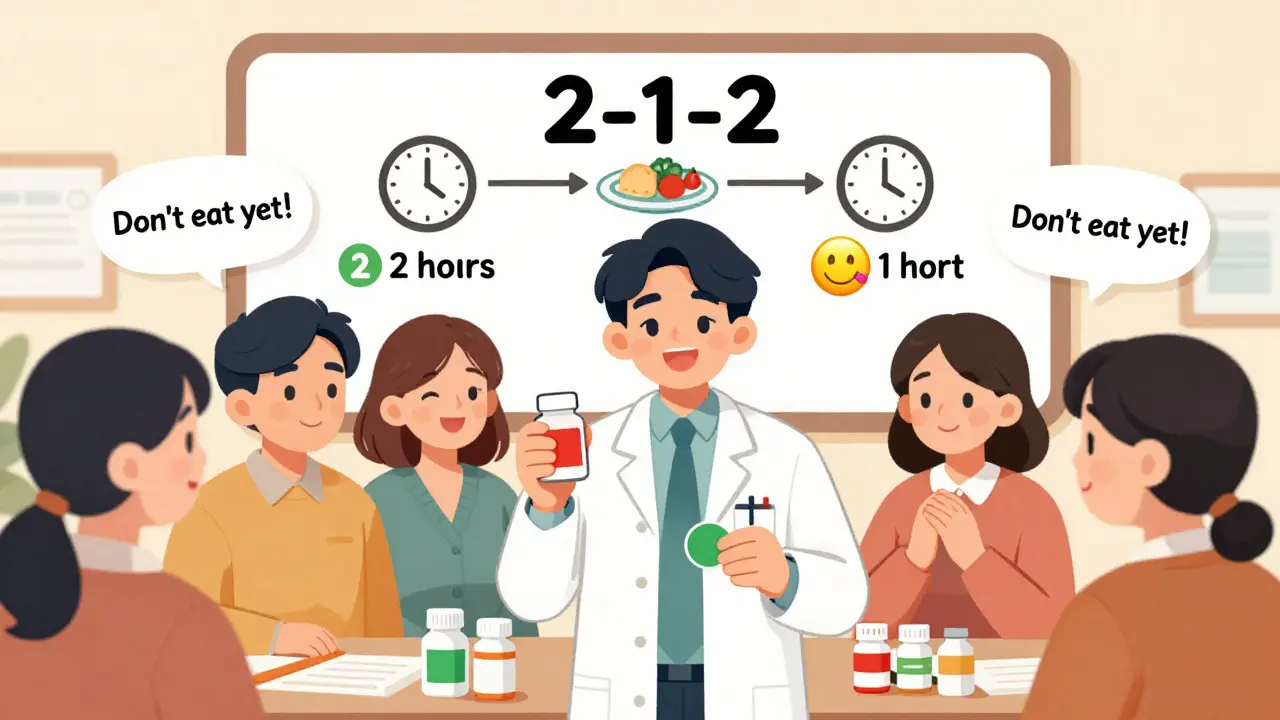
So how do you remember all this? The CDC’s 2023 guidelines recommend the 2-1-2 Rule:
- Take meds on an empty stomach: 2 hours after eating, or 1 hour before your next meal.
- Take meds with food: during or within 30 minutes of a meal.
A meal should be around 500-800 calories-not just a handful of crackers. That’s the amount used in FDA food-effect studies. A light snack won’t cut it. And if you’re taking multiple meds, space them out. Don’t take your levothyroxine at 7 AM and your statin at 7:05 AM. Wait 30-60 minutes between them. Many people think they’re being careful by taking everything at once. But that’s when interactions happen.
Real Stories, Real Consequences
On Reddit, a user named u/ThyroidWarrior shared that for two years, their TSH levels kept jumping around. They were doing everything right-taking Synthroid daily, getting blood tests. But they were taking it with coffee and cream. Once they switched to taking it at 4 AM with plain water and waiting 90 minutes before breakfast, their levels stabilized. No dose change. Just timing.
Another patient on Drugs.com said they’d been taking Nexium after lunch for months, wondering why their heartburn never improved. They didn’t know it had to be taken an hour before food. After switching, their symptoms vanished in two weeks.
And then there’s the flip side: u/IBDSurvivor on HealthUnlocked said taking mesalamine with food reduced their nausea from daily to once a month. That one change let them go back to work full-time.
What Pharmacies Are Doing to Help
Pharmacists are the most reliable source for food-timing advice. A 2021 JAMA study found 92% of pharmacists give clear instructions, compared to just 45% of doctors. That’s why you should always ask your pharmacist when you pick up a new prescription.
CVS and Walgreens now put color-coded stickers on bottles: red for “empty stomach,” green for “with food.” In a 2021 pilot study, this simple change boosted correct usage from 52% to 89%. Pharmacies also offer pill organizers labeled “AM: empty stomach” and “PM: with food.” A 2022 study in the Annals of Internal Medicine showed these improved adherence by 35%.
Apps like Medisafe and GoodRx now send alerts: “Take your levothyroxine in 15 minutes-don’t eat yet.” Their 2023 data shows a 28% drop in timing errors among users who turn on the alerts.
What’s Changing in the Future
Drug makers are starting to design pills that ignore food. Johnson & Johnson’s new Xarelto Advanced formula absorbs consistently whether you’ve eaten or not. University of Michigan researchers are testing nanoparticle versions of levothyroxine that bypass stomach pH entirely. Early results show 92% consistent absorption-fed or fasted.
The FDA is also moving to cut unnecessary food-effect testing for drugs that clearly don’t interact with food. That could speed up generic approvals. But experts warn: even with these advances, 75% of current medications still need careful timing. Understanding the basics isn’t going away.
Dr. Richard Hoppu from the University of Helsinki predicts we’ll soon have personalized food-timing algorithms-apps that track your eating habits and adjust your pill reminders based on your real gastric emptying rate. But until then, the old rules still apply.
What You Should Do Today
Don’t wait for a side effect or a lab result to tell you something’s wrong. Right now, open your medicine cabinet. Look at your prescriptions. Check the labels. Do they say “take on empty stomach” or “take with food”? If you’re unsure, call your pharmacy. Don’t assume your doctor told you. Don’t assume the pharmacist explained it. Ask again.
Write down your daily schedule: what you eat, when you take each pill. See where conflicts might happen. If you take levothyroxine and a calcium supplement, space them by at least 4 hours. If you take statins, avoid grapefruit juice completely. If you take ibuprofen, always eat something first.
Your meds aren’t magic. They’re chemicals. And chemicals respond to your body’s environment. Food changes that environment. Getting it right isn’t about being perfect-it’s about being consistent. One wrong timing can undo weeks of treatment. But one small change-taking your pill with food instead of on an empty stomach-could be the difference between feeling okay, and feeling like yourself again.
Can I take my medication with just a sip of water?
Yes, but only if the medication requires an empty stomach. Water doesn’t interfere with absorption. In fact, it’s required for most pills to dissolve properly. But if your pill says "take on an empty stomach," don’t add juice, coffee, milk, or even a small snack-even a cracker can trigger an interaction. Stick to plain water.
What if I forget and take my pill with food?
Don’t panic. Don’t double the dose. If you realize right away, wait 2 hours after eating, then take your next dose as scheduled. If it’s been more than an hour since you ate, skip the dose and wait until your next scheduled time. For drugs like levothyroxine or alendronate, missing one dose isn’t catastrophic-but making it a habit is. Talk to your pharmacist about how to get back on track.
Does it matter what kind of food I eat?
Yes. High-fat meals delay stomach emptying more than carbs or protein, which can affect time-sensitive drugs like levothyroxine. Calcium-rich foods (dairy, fortified orange juice) bind to antibiotics and thyroid meds. Grapefruit juice interferes with statins and some blood pressure drugs. Even fiber can slow absorption. For most drugs, a standard meal of 500-800 calories is what studies use. Avoid extremes unless your doctor says otherwise.
Why do some meds say "take with food" but don’t specify what food?
Because the goal is to reduce stomach upset or improve absorption, not to trigger a specific reaction. A light meal-like toast with peanut butter or a sandwich-is usually enough. For drugs like statins or duloxetine, any food that contains a little fat helps. You don’t need a full steak dinner. But avoid skipping food entirely. If you’re fasting, take the pill with a small snack like a banana or a handful of nuts.
Are over-the-counter meds affected by food too?
Absolutely. Many OTC painkillers like ibuprofen and naproxen cause stomach bleeding when taken empty. Antacids like Tums can interfere with antibiotics if taken too close together. Even vitamin C can affect how some iron supplements are absorbed. Just because it’s available without a prescription doesn’t mean it’s harmless. Always read the label. If it says "take with food," follow it.
Can I use a pill organizer for food-timing meds?
Yes, but only if it’s labeled correctly. Use organizers with separate AM/PM compartments and write "empty stomach" or "with food" on each slot. Don’t just put all your pills in one compartment. A 2022 study showed labeled organizers improved adherence by 35%. Some pharmacies even offer pre-labeled ones. If you’re on 5+ meds, ask your pharmacist for help setting one up.
16 Comments
Write a comment
More Articles
Atorvastatin and Erectile Dysfunction: Exploring the Possible Link
Explore whether atorvastatin contributes to erectile dysfunction, review clinical studies, and learn how to manage any sexual side effects safely.

Thomas Anderson
December 16, 2025 AT 16:44Just took my levothyroxine with coffee this morning. Guess I’m doing it wrong. 😅