
Ever wondered why two men with low testosterone can feel completely different? The answer often lies in the hypogonadism types they have. Knowing whether the problem starts in the testicles or higher up in the brain can change everything from testing to treatment.
Key Takeaways
- Hypogonadism is a hormone deficiency that can originate in the testes (primary) or in the brain’s pituitary/hypothalamic axis (secondary).
- Primary and secondary forms have distinct causes, lab patterns, and treatment pathways.
- Accurate diagnosis relies on measuring testosterone together with gonadotropins - luteinizing hormone (LH) and follicle‑stimulating hormone (FSH).
- Genetic syndromes like Klinefelter and Turner are classic examples of primary hypogonadism.
- Pituitary tumors, prolonged steroid use, and high‑dose opioids are leading culprits of secondary hypogonadism.
What is Hypogonadism a condition where the body produces insufficient sex hormones, mainly testosterone in men, due to problems with the gonads or the signaling centers in the brain?
In simple terms, hypogonadism means the body’s hormone factory isn’t churning out enough testosterone. Testosterone drives muscle mass, libido, bone density, mood, and red blood cell production. When levels dip, you might notice fatigue, reduced sexual drive, loss of muscle, or even anemia.
The condition isn’t one‑size‑fits‑all. The root cause determines the label, the lab clues, and the best way to fix it.
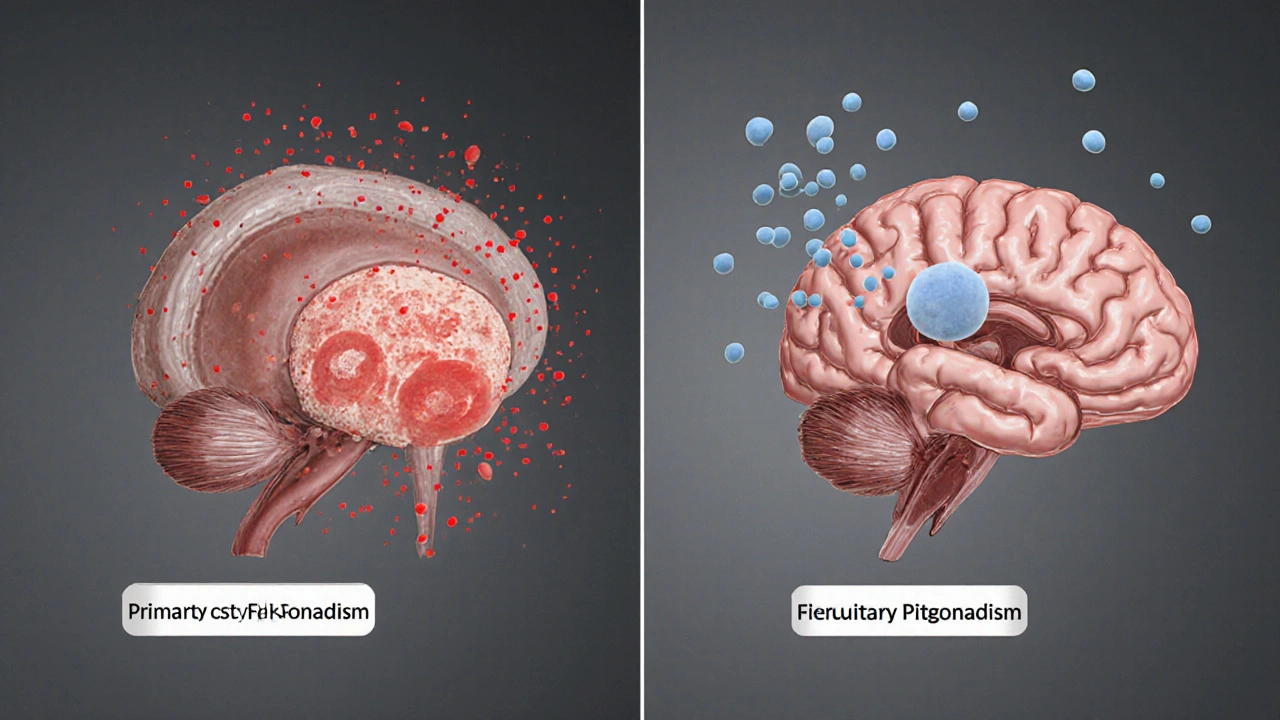
Primary (Testicular) Hypogonadism also called hypergonadotropic hypogonadism; the testes themselves are damaged or underdeveloped, leading to low testosterone despite high stimulating hormones
With primary hypogonadism, the testicles can’t respond to signals from the brain. The pituitary gland notices the low testosterone and cranks up production of LH and FSH, so blood tests typically show high gonadotropins.
Common causes include:
- Genetic disorders - Klinefelter syndrome a male chromosomal condition (47,XXY) that impairs testicular development
- Physical injury or surgery affecting the testes
- Infections such as mumps orchitis
- Radiation or chemotherapy that damages germ cells
- Autoimmune orchitis
Secondary (Pituitary‑Hypothalamic) Hypogonadism also known as hypogonadotropic hypogonadism; the brain’s signaling centers fail to stimulate the testes, resulting in low testosterone with low or normal LH and FSH
Here the problem isn’t the testicles but the command center - the hypothalamus and pituitary gland. If they don’t release enough gonadotropins, the testes stay idle.
Typical triggers are:
- Pituitary tumor a benign growth that can compress or disrupt hormone‑secreting cells
- Prolonged use of glucocorticoids or high‑dose opioids
- Severe systemic illness (e.g., HIV, chronic kidney disease)
- Congenital defects affecting the hypothalamus - Kallmann syndrome a rare condition where the hypothalamus lacks gonadotropin‑releasing hormone (GnRH) neurons
- Trauma or surgery to the brain or pituitary stalk
Mixed or Combined Forms
Sometimes both the testes and the brain are partially impaired. Mixed hypogonadism can arise after chemotherapy that damages testicular cells while also disrupting the hypothalamic‑pituitary axis. Lab values may show intermediate or fluctuating LH/FSH levels, so a comprehensive endocrine work‑up is crucial.
How Doctors Diagnose the Different Types
The diagnostic roadmap starts with a detailed history and physical exam, followed by targeted labs:
- Morning total Testosterone the primary male sex hormone; low levels (<300 ng/dL) suggest hypogonadism measured before 10am.
- Serum Luteinizing hormone (LH) stimulates testosterone production in Leydig cells and Follicle‑stimulating hormone (FSH) supports sperm production in Sertoli cells. High levels point to primary hypogonadism; low/normal levels hint at secondary.
- Prolactin level - elevated prolactin can suppress GnRH and mimic secondary hypogonadism.
- Sex hormone‑binding globulin (SHBG) and free testosterone - useful when total testosterone is borderline.
- Imaging: MRI of the pituitary for suspected tumors; scrotal ultrasound for testicular atrophy or lesions.
- Genetic testing when a syndrome is suspected (e.g., karyotype for Klinefelter, sequencing for Kallmann).
Interpreting the hormone panel in context is the key to labeling the correct type.
Treatment Strategies Tailored to the Type
Once the type is clear, therapy becomes more focused.
- Primary hypogonadism: Direct testosterone replacement (gels, patches, injections) is usually first‑line because the testes can’t produce enough on their own. In younger men desiring fertility, gonadotropin therapy (hCG ± FSH) can stimulate natural testosterone and sperm production.
- Secondary hypogonadism: Treat the underlying cause whenever possible - surgery for a pituitary adenoma, tapering off opioids, or correcting hyperprolactinemia with dopamine agonists. If the axis remains suppressed, testosterone replacement is added, but gonadotropin therapy may be more physiological if fertility is a goal.
- Mixed cases: A combination approach-address any reversible brain factors, then supplement testosterone while monitoring testicular response.
Monitoring involves repeat hormone panels every 3‑6months, symptom questionnaires, bone density scans, and semen analysis if fertility matters.

Comparison Table: Primary vs. Secondary Hypogonadism
| Feature | Primary (Testicular) | Secondary (Pituitary‑Hypothalamic) |
|---|---|---|
| Site of defect | Testes | Hypothalamus or pituitary gland |
| LH & FSH levels | High (hypergonadotropic) | Low or normal (hypogonadotropic) |
| Common causes | Klinefelter syndrome, orchitis, radiation | Pituitary adenoma, opioids, Kallmann syndrome |
| Treatment focus | Testosterone replacement or gonadotropins for fertility | Address underlying brain issue; testosterone if needed |
| Typical age of presentation | Adolescence to late adulthood | Can appear at any age, often linked to medication or disease |
Practical Checklist for Patients and Clinicians
- Document symptoms: fatigue, libido, muscle loss, mood changes.
- Order morning total testosterone, LH, FSH, prolactin.
- If testosterone < 300ng/dL, repeat test to confirm.
- Interpret LH/FSH pattern to decide primary vs. secondary.
- Consider MRI of pituitary if secondary signs appear.
- Screen for genetic syndromes when testicular atrophy or atypical features are present.
- Discuss fertility goals early; choose hCG/FSH or testosterone accordingly.
- Set follow‑up schedule: labs every 3-6months, symptom review each visit.
Frequently Asked Questions
Can lifestyle changes reverse hypogonadism?
In secondary hypogonadism caused by obesity, excessive alcohol, or chronic stress, weight loss, better sleep, and reduced alcohol can improve hormone levels. However, structural damage to the testes or a tumor usually requires medical intervention.
Is testosterone therapy safe for older men?
Short‑term therapy is generally well‑tolerated, but clinicians monitor hematocrit, prostate‑specific antigen, and cardiovascular risk. The decision balances symptom relief with potential side effects.
What’s the difference between total and free testosterone?
Total testosterone includes the hormone bound to SHBG and albumin, while free testosterone is the biologically active fraction. In cases of abnormal SHBG (e.g., thyroid disease), free testosterone gives a clearer picture.
Can men with primary hypogonadism ever father children?
Yes, with gonadotropin therapy (hCG ± FSH) many men can stimulate natural testosterone production and restore sperm output, offering a more natural path to fertility than sperm banking.
Why is LH high in primary hypogonadism?
When testicular testosterone drops, the pituitary senses the gap and releases more LH to try to boost production. The testes can’t respond, so LH stays elevated.
18 Comments
Write a comment
More Articles
Fludrocortisone and Skin Health: Understanding Potential Side Effects
Learn how fludrocortisone can affect your skin, recognize common side effects like edema, acne, and hyperpigmentation, and get practical tips to manage them safely.

Minoxytop vs Other Hair‑Loss Treatments: Pros, Cons & Best Picks
A side‑by‑side review of Minoxytop vs finasteride, PRP, laser therapy, transplants and natural options, with a comparison table, tips and FAQs.

Patient Safety Goals in Medication Dispensing and Pharmacy Practice: How to Prevent Errors and Save Lives
Discover the real-world safety goals that prevent medication errors in pharmacies and hospitals. Learn how barcode scanning, high-alert drug controls, and system redesign-not just training-save lives.
Kristen Woods
October 8, 2025 AT 13:41Indeed, the dichotomy between primary and secondary hypogonadism is a theatrical drama of endocrinology, each with its own cascade of hormonal missteps. The lab values, when interpreted correctly, definately reveal which organ-testis or hypothalamus-has betrayed its duty. Let us not overlook the profound impact this distinction has on therapeutic strategy.