
What Is Aspirin-Exacerbated Respiratory Disease?
Aspirin-Exacerbated Respiratory Disease, or AERD, is a chronic condition that affects adults who have three things happening at once: asthma, nasal polyps, and severe breathing reactions to aspirin or common NSAIDs like ibuprofen and naproxen. It’s not just an allergy-it’s a full-body inflammatory disorder that starts in the sinuses and spreads to the lungs. First noticed in the 1920s and later fully mapped out in the 1960s by Dr. Max Samter, it’s often called Samter’s Triad because of those three classic signs.
Most people develop AERD between ages 20 and 50. Women are slightly more likely to get it than men, making up about 60% of cases. Around 7% of all adult asthmatics have AERD, but if you already have nasal polyps, your chance jumps to 14%. That’s not a small risk-it means if you’ve had polyps removed more than once and still struggle with breathing, AERD could be the hidden cause.
Why Do Aspirin and NSAIDs Trigger Reactions?
It’s not that your body hates aspirin. It’s that your body’s chemistry is broken in a very specific way. In AERD, the normal pathway that breaks down fats in your body-called arachidonic acid metabolism-gets stuck. Instead of making harmless byproducts, your body overproduces something called cysteinyl leukotrienes. These are powerful inflammatory chemicals that swell your nasal passages, tighten your airways, and flood your lungs with mucus.
When you take aspirin or another NSAID, you block an enzyme called COX-1. That sounds helpful, right? But in AERD, blocking COX-1 doesn’t reduce inflammation-it makes the problem worse. The blocked pathway forces even more leukotrienes to be made. Within 30 to 120 minutes, you might feel your nose clog, your chest tighten, or your breathing turn shallow. Some people even get hives or low blood pressure. These reactions don’t happen in regular asthma. That’s why AERD needs a different kind of diagnosis.
How Is AERD Diagnosed?
There’s no single blood test or scan that confirms AERD. Diagnosis relies on your medical history and, when needed, a controlled challenge test. Doctors look for the full triad: asthma confirmed by lung function tests, nasal polyps seen on imaging or during exam, and a clear pattern of breathing problems after taking aspirin or NSAIDs.
If your history is unclear-maybe you’ve never taken aspirin before, or you avoid all painkillers-you’ll need a supervised aspirin challenge. This isn’t something you do at home. It’s done in a hospital or allergy clinic with emergency equipment ready. You start with a tiny dose of aspirin-20 to 30 milligrams-and every 90 to 120 minutes, the dose doubles. You’re watched closely for wheezing, nasal congestion, or drops in lung function. The test ends at 325 mg, or sooner if symptoms appear. About 85% of people with suspected AERD will react during this test.
Lab tests can support the diagnosis. Blood eosinophils (a type of white blood cell) are often above 500 cells per microliter. Urine tests for leukotriene E4, a marker of inflammation, are elevated in nearly 9 out of 10 patients during active disease. These aren’t diagnostic on their own, but when they line up with your symptoms, they confirm the picture.

What Happens If You Just Avoid Aspirin and NSAIDs?
Many people think avoiding NSAIDs will fix their AERD. It won’t. Avoiding aspirin might prevent the sudden attacks, but it doesn’t stop the slow, steady worsening of your polyps or asthma. The inflammation keeps going, even without triggers. That’s why most patients still need surgery multiple times and still struggle with daily breathing problems.
Medications help, but they’re not a cure. High-dose steroid nasal rinses-like 50 to 100 mg of budesonide in saline, used twice daily-can shrink polyps by 30 to 40% in just eight weeks. Intranasal sprays like fluticasone help with congestion. For asthma, a combination inhaler with corticosteroids and a long-acting beta agonist improves lung function by 15 to 20% in most people.
Leukotriene blockers like montelukast (Singulair) are often tried, but they only help 15% of AERD patients significantly. Zileuton works better-it cuts leukotriene levels by 75%-but it requires taking four pills a day and monitoring liver function. Biologics like dupilumab and mepolizumab are game-changers for severe cases. Dupilumab reduces polyp size by over half in 16 weeks and improves smell in 8 out of 10 patients. But these drugs cost thousands per month, and insurance doesn’t always cover them.
Aspirin Desensitization: The Most Effective Long-Term Treatment
If you’ve had sinus surgery and still get polyps back, or if your asthma won’t stabilize, aspirin desensitization is your best option. This isn’t a one-time fix-it’s a lifelong management strategy that changes how your body responds to inflammation.
The process starts with the same challenge test used for diagnosis. But instead of stopping when you react, doctors keep giving you aspirin until you tolerate a full 325 mg dose. Once you can handle that, you start taking 650 mg twice daily-every day, no exceptions. This doesn’t just prevent reactions. It rewires your immune system. After six months, most patients see fewer sinus infections, smaller polyps, and better lung function.
Studies show that after desensitization, the need for oral steroids drops from over four bursts per year to just one. Polyp recurrence after surgery falls from 85% to 35% in two years. Smell returns for most people-the University of Pennsylvania smell test scores jump from 12 to 24 out of 40. For many, it’s the first time in years they can smell coffee, rain, or their child’s shampoo.
But it’s not easy. Missing two or three days of aspirin means you have to go through the whole desensitization process again. About 68% of patients who skip doses need to restart. Stomach issues like ulcers or bleeding happen in 22% of long-term users. That’s why you need a doctor who knows how to manage this safely.
Why Surgery Alone Isn’t Enough
Functional endoscopic sinus surgery (FESS) is common for AERD patients. It opens up blocked sinuses and removes polyps. Most people feel better right after-breathing improves, pressure eases, sleep gets better. But without desensitization, polyps come back fast. In 18 months, 60 to 70% of patients need another surgery.
When you combine FESS with aspirin desensitization, recurrence drops to 25 to 30% over two years. That’s a 65% reduction in polyp regrowth compared to surgery alone. Experts agree: if you’re having sinus surgery for AERD, you should be offered desensitization before you leave the hospital.
But not all doctors know this. Only 18% of U.S. allergists feel confident managing AERD. There are only about 35 specialized centers nationwide. If your doctor hasn’t mentioned desensitization, ask for a referral to an AERD specialist. Telemedicine has helped-many centers now offer virtual consultations to guide local providers.

Who Shouldn’t Try Desensitization?
Desensitization isn’t for everyone. If you have unstable heart disease, active peptic ulcers, or a history of severe gastrointestinal bleeding, it’s too risky. If you can’t commit to taking aspirin every single day, it won’t work. About 15% of potential candidates are turned away for these reasons.
Some people can’t tolerate the aspirin challenge. About 32% of patients report high anxiety or severe symptoms during the test. But most get through it with support. If you’re nervous, ask about pre-medication with antihistamines or steroids to reduce the reaction.
Cost is another barrier. Biologics like dupilumab can cost over $30,000 a year. Even aspirin desensitization requires multiple visits and follow-ups. But the long-term savings are real. Each revision sinus surgery costs around $18,500. Desensitization saves money by preventing those surgeries-and it improves your quality of life in ways no number can fully capture.
What’s Next for AERD Treatment?
The field is moving fast. New drugs like tipelukast (MN-001), which blocks two inflammation pathways at once, are in early trials and show promise. Combining dupilumab with aspirin therapy gives even better results than either alone. FDA guidelines are now standardizing how desensitization is done, so more clinics can offer it safely.
But access remains unequal. Only 22% of rural AERD patients live within 100 miles of a specialist. Insurance still fights coverage for biologics. Many patients report having to pay out of pocket or wait months for appointments.
Still, the outlook is better than ever. AERD used to be a life sentence of repeated surgeries and worsening asthma. Now, with the right care, many people live symptom-free for years. The key is recognizing the triad early, getting the right diagnosis, and choosing the full treatment plan-not just avoiding aspirin, but actively retraining your body to stop fighting itself.
Real Patient Stories
On patient forums like AERD Warriors and Reddit’s r/SamtersTriad, stories repeat: years of blocked sinuses, lost sense of smell, emergency room visits for asthma attacks. Then, after desensitization: "I smelled my wife’s perfume for the first time in 12 years." "I stopped using my rescue inhaler." "I went on a hike without stopping to catch my breath." One woman in Ohio, after her third sinus surgery, started aspirin desensitization. Two years later, her polyps were gone. Her lung function improved. She stopped taking oral steroids. She says, "I didn’t know I could feel this normal again." These aren’t outliers. They’re the new standard-for those who get the right care.
12 Comments
Write a comment
More Articles

Sunburn and Skin Cancer: Essential Facts & Prevention
Explore how sunburn damages skin DNA, raises skin‑cancer risk, and learn practical steps to prevent and detect melanoma, basal and squamous cell cancers.
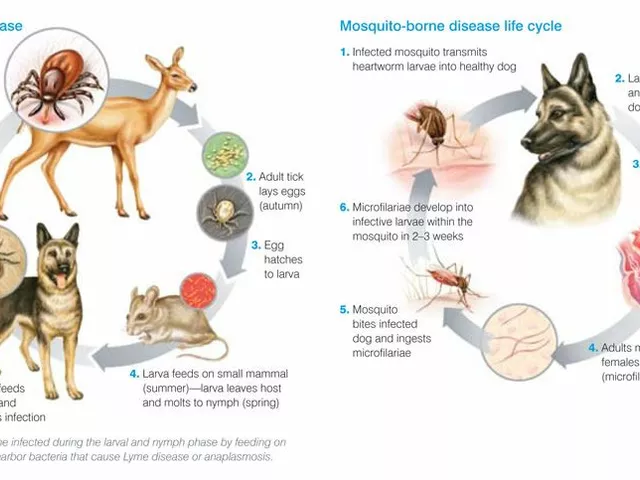
Tick Fever: What You Need to Know About This Dangerous Disease
Tick Fever, also known as Tick-Borne Disease, is a serious illness transmitted by ticks. It's crucial to be aware that this disease can have severe health implications including fever, headache, and fatigue, and in some cases can even be fatal. Early detection and treatment are absolutely vital. It's also important to take steps in preventing tick bites, such as using repellents and wearing appropriate clothing when in tick-infested areas. Stay safe out there, folks!

Ibrahim Yakubu
December 7, 2025 AT 11:41I’ve seen this in Lagos clinics-patients with polyps and asthma, told it’s just allergies. No one connects it to NSAIDs. I had a cousin who collapsed after ibuprofen. They thought it was a heart thing. Turned out to be AERD. Took three ER visits and a neurologist to finally get the right diagnosis. The leukotriene urine test? That’s the key. Nobody runs it unless you push. Don’t wait for your doctor to know. Bring the paper. Print it. Make them read it.