
Opioid Side Effect Management Guide
Opioid side effects like constipation, drowsiness, and nausea are common but manageable. Select the side effect you're experiencing to get personalized guidance on how to handle it.
Constipation Management
Opioids slow down gut movement, causing constipation that typically doesn't improve over time. Start laxatives on day one as recommended by guidelines.
When to seek immediate help:
- Severe abdominal pain
- Rectal bleeding
- Not having a bowel movement for 3+ days despite laxatives
Recommended Treatment
Start with a combination of:
- Stimulant laxative (e.g., senna)
- Osmotic agent (e.g., polyethylene glycol)
Drink plenty of water and eat fiber-rich foods. Light exercise can help as well.
When opioids are prescribed for severe pain-after surgery, for cancer, or following a major injury-they work. But they also bring unwanted guests: constipation, drowsiness, and nausea. These aren’t rare or mild. They’re common, predictable, and often ignored until they make life harder than the pain itself.
Constipation: The One Side Effect That Never Goes Away
If you’re on opioids long-term, you will likely get constipated. Not maybe. Not sometimes. Constipation happens to nearly everyone. It’s not a sign you’re eating wrong or not drinking enough water. It’s how opioids work.
Opioids bind to receptors in your gut, slowing down the natural muscle contractions that move food through your system. That means stool sits longer, water gets sucked out, and you’re stuck. Unlike drowsiness or nausea, which often fade after a few days, constipation sticks around as long as you’re on the drug.
Doctors used to wait until patients complained before acting. Now, guidelines from the American Academy of Family Physicians say: start laxatives on day one. Don’t wait. Prophylactic treatment isn’t optional-it’s standard. A mix of a stimulant laxative like senna and an osmotic agent like polyethylene glycol works best. These help keep things moving without killing the pain relief.
For those who don’t respond, newer options like methylnaltrexone (Relistor) or naloxegol (Movantik) exist. These drugs block opioid effects in the gut but don’t cross into the brain, so your pain control stays intact. They’re not cheap, but for someone stuck for weeks, they’re life-changing.
Drowsiness: When Your Brain Feels Like It’s Underwater
At first, opioids make you sleepy. Not just tired. Like your thoughts are thick, your eyelids heavy, and even simple decisions feel like climbing a hill. Between 20% and 60% of new users experience this. It’s not laziness. It’s your brain’s response to opioids binding to receptors in the central nervous system.
Most people adjust within a week or two. Tolerance builds. The fog lifts. But for 10-15% of long-term users, the drowsiness doesn’t fade. It becomes a barrier to work, driving, or even caring for kids. Mental fog can mimic memory loss or confusion, especially in older adults or those with existing cognitive issues.
Doctors often suggest adjusting the dose or timing-taking the pill at night if possible. Avoid mixing opioids with alcohol, benzodiazepines like Xanax, or sleep aids. That combo can slow breathing to dangerous levels. If drowsiness won’t quit, some providers consider stimulants like methylphenidate (Ritalin), but evidence is thin and side effects like anxiety or high blood pressure can make it risky.
The key? Don’t push through it. If you’re nodding off at your desk or almost falling asleep driving, talk to your provider. There’s no shame in needing a lower dose or a different pain plan.
Nausea: Why Your Stomach Feels Like It’s Revolting
Nausea hits about one in four people starting opioids. It’s not just feeling queasy-it’s the urge to throw up, sometimes for days. This happens because opioids trigger the brain’s vomiting center and slow stomach emptying. It’s not about food. It’s pharmacology.
For most, nausea fades after 3 to 7 days. But for 10% of long-term users, it lingers. That’s enough to make people skip doses, stop taking the medication entirely, or worse-turn to illegal drugs just to feel normal.
Anti-nausea meds are the go-to fix. Dopamine blockers like metoclopramide or prochlorperazine are usually tried first. If those don’t work, serotonin blockers like ondansetron (Zofran) or antihistamines like promethazine may help. Sometimes, switching to a different opioid reduces nausea-morphine tends to be worse than oxycodone, for example.
Important note: stopping opioids suddenly can also cause nausea, vomiting, and diarrhea. That’s withdrawal. The FDA warns that abrupt discontinuation can lead to uncontrolled pain, panic, and even suicide risk. If you want off opioids, work with your doctor on a slow, safe taper.
Why Managing Side Effects Matters More Than You Think
These three side effects-constipation, drowsiness, nausea-are more than just annoyances. They’re why people stop taking their meds. And when they stop, pain comes back. Worse, some turn to street drugs to replace what they lost. The CDC reports that over two-thirds of people who misused prescription opioids did so because they couldn’t manage their pain or side effects.
It’s not about being weak. It’s about biology. Opioids were never meant to be taken for years without support. The goal isn’t just to relieve pain-it’s to help people live. That means treating the side effects as seriously as the pain itself.
Doctors who skip this step aren’t being negligent-they’re often overwhelmed. But patients shouldn’t have to beg for laxatives or anti-nausea pills. These should be part of every opioid prescription plan from day one.
What You Can Do Right Now
- If you’re starting opioids, ask for a laxative prescription before you leave the clinic. Don’t wait until you’re backed up.
- Drink plenty of water, eat fiber-rich foods, and move daily-even a short walk helps.
- If you feel drowsy, don’t drive or operate machinery. Tell your doctor. There’s no need to suffer in silence.
- If nausea hits, try ginger tea or small, bland meals. Keep anti-nausea meds on hand if prescribed.
- Never stop opioids cold turkey. Talk to your provider about a taper plan if you want to stop.
There’s no perfect opioid. But there are better ways to use them. When side effects are managed proactively, people get their pain under control without losing their quality of life.
When to Seek Help
Call your doctor if:
- You haven’t had a bowel movement in 3 days despite laxatives.
- You’re so drowsy you can’t stay awake during the day.
- Nausea lasts more than a week or you’re vomiting repeatedly.
- You feel confused, dizzy, or have trouble breathing.
These aren’t normal. They’re red flags. Your body is telling you something needs to change.
Is constipation from opioids permanent?
No, but it lasts as long as you take opioids. Unlike drowsiness or nausea, which often fade, constipation doesn’t improve with tolerance. That’s why doctors recommend starting laxatives right away. There are effective treatments like methylnaltrexone or naloxegol that target the gut without affecting pain relief.
Can I just stop taking opioids if the side effects are too bad?
No. Stopping suddenly can cause withdrawal symptoms like nausea, vomiting, diarrhea, anxiety, and severe pain. In rare cases, it can lead to suicidal thoughts. Always work with your doctor to create a slow, controlled taper plan. They can help you switch to a different medication or use non-opioid pain treatments instead.
Why do opioids make me so sleepy?
Opioids affect brain areas that control alertness and wakefulness. They slow down your central nervous system, which can cause drowsiness, mental fog, and reduced reaction time. This usually improves after a few days as your body adjusts. If it doesn’t, your dose may be too high, or you might need a different pain medication.
Are there opioids that don’t cause nausea?
All opioids can cause nausea, but some are less likely than others. Oxycodone and tramadol tend to cause less nausea than morphine or hydromorphone. But it varies by person. If nausea is a problem, your doctor might try switching you to a different opioid or adding an anti-nausea medication like ondansetron.
Can I use over-the-counter laxatives with opioids?
Yes, and you should. Most experts recommend starting a combination of a stimulant laxative (like senna) and an osmotic agent (like polyethylene glycol) from the first day of opioid use. Over-the-counter options work fine for most people. If they don’t help after a week, talk to your doctor about prescription options like methylnaltrexone.
Do opioid side effects mean I’m addicted?
No. Side effects like constipation, drowsiness, and nausea are physical reactions to the drug, not signs of addiction. Addiction involves compulsive use despite harm, cravings, and loss of control. You can have all these side effects and still take your medication exactly as prescribed. But if you’re using more than prescribed or seeking opioids for reasons other than pain, that’s a red flag.
What Comes Next?
The future of pain management isn’t just about stronger opioids. It’s about smarter ones. Researchers are developing drugs that target pain pathways without triggering the receptors that cause nausea or constipation. Some are even exploring non-opioid alternatives like nerve blocks, physical therapy, and certain antidepressants that help with chronic pain.
For now, if you’re on opioids, don’t accept side effects as normal. Talk to your doctor. Ask for a plan. You deserve to manage your pain without losing your daily life to constipation, sleepiness, or vomiting. You’re not alone-and there are better ways.
14 Comments
Write a comment
More Articles
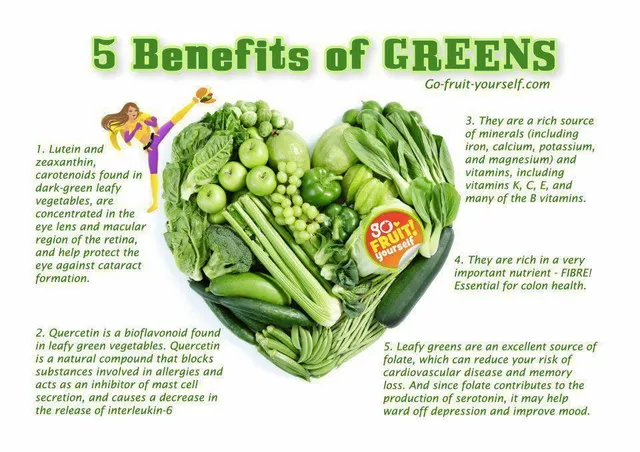
Folate Deficiency and Eye Health: What You Need to Know
As a blogger, I recently came across an important topic concerning eye health - folate deficiency. Folate, also known as vitamin B9, plays a crucial role in maintaining our overall well-being, including our precious eyesight. A deficiency in folate can lead to various eye problems, such as macular degeneration and optic neuropathy. To prevent these issues, it's essential to consume a balanced diet rich in leafy greens, beans, and fortified cereals. So, let's take care of our eyes by ensuring we get enough folate in our daily diets!

Tom Shepherd
November 28, 2025 AT 12:31Opioid constipation is the worst part of pain management and nobody talks about it like it’s a normal part of the deal. I was on oxycodone for six months after my back surgery and I swear I forgot what a normal bowel movement felt like. Started senna and MiraLAX day one like the article said and it was a game changer. Still had to drink a gallon of water a day but at least I wasn’t screaming in the bathroom for an hour.