
When you pick up a prescription, the label looks like a tiny instruction manual written in code. For regular pills, it’s simple: take one in the morning, one at night. But when you see ER, XR, SR, or CR after the drug name, things change. These aren’t just extra letters. They’re life-or-death signals. If you misread them, you could end up taking too much too fast - or not enough at all.
What Extended-Release Really Means
Extended-release medications are built to let the drug leave your body slowly. Instead of one big burst, it trickles out over hours. That’s why you only need to take them once or twice a day, instead of every 4 to 6 hours like immediate-release versions. Think of it like a slow-burning candle versus a match. One gives steady light. The other flares up and dies fast.The science behind it isn’t magic. It’s engineering. Some pills use a polymer shell that dissolves over time. Others have tiny beads inside a capsule, each coated to release at a different pace. A few use osmotic pumps - like a tiny water-powered timer - to push the drug out steadily. All of them rely on one rule: don’t break the system.
Decoding the Suffixes on Your Label
You’ll see these letters after the drug name:- ER = Extended Release
- XR = eXtended Release
- SR = Sustained Release
- CR = Controlled Release
- CD = Continuous Delivery
They all mean roughly the same thing: this isn’t a regular pill. But here’s the catch - the same letter doesn’t always mean the same thing. Two different drugs labeled “ER” can release their medicine in completely different ways. For example, Concerta uses an osmotic pump to release dextroamphetamine over 12 hours. A generic “extended-release methylphenidate” might use a matrix system that dissolves slowly. Both are ER. Both work. But they’re not interchangeable.
That’s why you’ll often see the brand name in parentheses after the generic name: metoprolol succinate 24 hour extended release (Toprol XL). The “24 hour” part is critical. It tells you how long the drug is designed to last. Some extended-release pills last 12 hours. Others last 24. Taking a 12-hour pill twice a day when you think it’s 24-hour? That’s a mistake.
The One Rule You Must Never Break
If you see “DO NOT CRUSH, SPLIT, OR CHEW” on your label - don’t do it. Not even a little.Crushing a 24-hour extended-release tablet turns it into a time bomb. All the medicine inside rushes out at once. A single 60mg extended-release oxycodone tablet, when crushed, can deliver a dose equal to six immediate-release pills. That’s enough to stop your breathing. The FDA has logged over 1,200 serious adverse events between 2018 and 2022 from people crushing or snorting these pills.
Even splitting can be dangerous. Some pills are designed to release from the outside in. Cut them in half, and you expose the inner core - which might be packed with a full day’s dose. A pharmacist in Birmingham reported three cases last year alone of patients who split their extended-release blood pressure pills, thinking they were saving money. Two ended up in the hospital with dangerously low heart rates.

When and How to Take It
Timing matters more than you think. Some extended-release meds work best in the morning. Others need to be taken at night.Take Niaspan (niacin extended-release) in the evening. It causes flushing - that hot, red feeling on your face and chest. Taking it at bedtime means you’re asleep when it hits. Take Adderall XR in the morning. If you take it at night, you’ll be wired for hours. One user on Drugs.com wrote: “I took Adderall XR at night thinking it would last all day and kept me awake for 36 hours.” That’s not a side effect - that’s a misread label.
Check the “Directions” section on your label. It doesn’t just say “take once daily.” It says when. “Take in the morning with food.” “Take at bedtime.” “Take on an empty stomach.” These aren’t suggestions. They’re part of how the drug works. Food can delay absorption. Stomach acid can break down the coating. The timing is built into the design.
What’s in the Inactive Ingredients
The “Inactive Ingredients” list on your label isn’t filler. It’s the engineering blueprint. These are the polymers, waxes, and coatings that control how the drug releases. If you have a rare allergy - say, to lactose or a specific dye - it could be hiding here. The FDA keeps a database of these ingredients, and every approved extended-release product must list them.Some extended-release capsules are designed to pass through your gut whole. You might see the empty shell in your stool. That’s normal. The drug was already absorbed. Don’t panic. Don’t think you didn’t get your dose. That shell is just the delivery system - like the empty husk of a seed after the plant has grown.
Why Generic Versions Can Be Risky
Generic drugs are cheaper. That’s good. But with extended-release, not all generics are equal.Three different companies make extended-release diltiazem - a heart medication. All are labeled “24-hour extended release.” But their release profiles are different. One might peak at 8 hours. Another at 12. One might work better with food. The FDA says they’re not interchangeable. Your doctor chose one for a reason. Switching without telling them could throw off your rhythm.
Even if two generics have the same name, they might use different release tech. One might be a matrix tablet. Another might be coated beads. Same drug. Different results. That’s why your pharmacist asks if you’ve switched brands before.
What to Do When You’re Confused
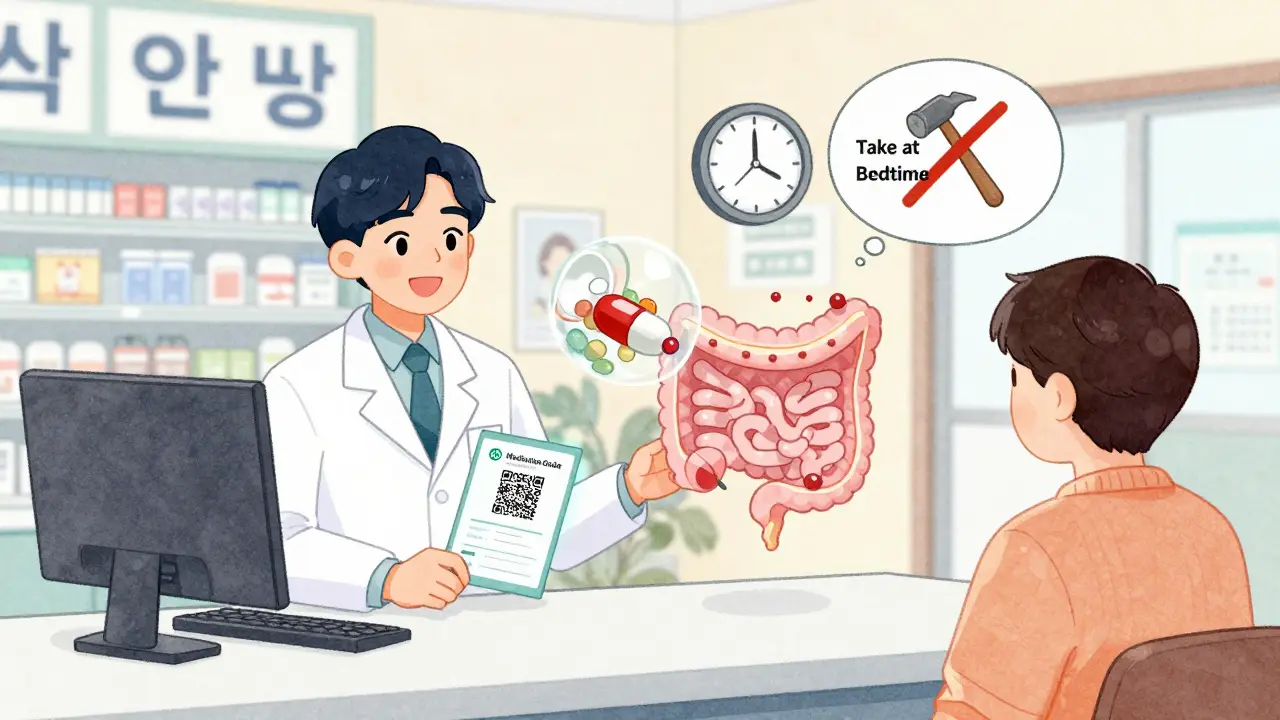
If the label doesn’t make sense - or if you’re unsure - don’t guess.- Ask your pharmacist. Say: “Can you explain how this pill works and why I shouldn’t crush it?”
- Use the Medication Guide. By law, pharmacies must give you a printed guide for high-risk extended-release drugs like opioids or ADHD meds. Read it.
- Scan the QR code. Newer labels have them. They link to short videos showing how to take the pill and what to avoid.
- Use the “teach-back” method. After your pharmacist explains, say: “So if I crush this, it could make me sick. I take it once a day in the morning, and I never split it.” If you can say it back right, you got it.
Over 42% of adults over 65 misunderstand “extended release” to mean “longer-lasting effect” - but miss the “do not crush” warning. That’s not just confusion. It’s a safety gap. You’re not alone. But you can close it.
The Bigger Picture
Extended-release medications are one of the biggest advances in modern pharmacy. They help people with chronic conditions - high blood pressure, diabetes, depression - stick to their treatment. Studies show adherence improves by up to 22% with once-daily dosing. That means fewer hospital visits. Fewer complications.But that only works if you take them right. The system is designed to be safe. But it only works if you don’t break it. Your label isn’t just instructions. It’s your protection.
What does ER, XR, or SR mean on a prescription label?
ER stands for Extended Release, XR for eXtended Release, and SR for Sustained Release. All mean the medication is designed to release slowly over time - usually 12 or 24 hours - so you don’t need to take it as often. But these terms don’t mean the same thing across all drugs. Different manufacturers use different technologies, so even two pills with the same label can work differently.
Can I split or crush an extended-release pill if it’s too big to swallow?
No. Crushing or splitting an extended-release pill releases the entire dose at once. This can cause a dangerous spike in drug levels, leading to overdose, heart problems, or even death. If you have trouble swallowing pills, ask your doctor or pharmacist for a liquid version, a different formulation, or a smaller tablet. Never force it.
Why does my extended-release medication say "take at bedtime"?
Some extended-release drugs are timed to work best when taken at night. For example, Niaspan (niacin) causes flushing - a hot, red feeling - and taking it at bedtime means you’re asleep when it happens. Other drugs, like certain blood pressure meds, lower your blood pressure during sleep, helping prevent morning spikes. Always follow the timing on the label - it’s part of how the drug works.
Are generic extended-release drugs the same as brand names?
Not always. While generics must contain the same active ingredient, the release mechanism can differ. For example, three different extended-release versions of diltiazem exist, and they’re not interchangeable. Switching without your doctor’s approval can change how the drug works in your body. Always check with your pharmacist before switching brands.
I saw the empty shell of my pill in the toilet. Did I not absorb the medicine?
That’s normal. Many extended-release pills are designed to pass through your digestive system intact after releasing the drug. The shell you see is just the delivery system - like the husk of a seed. The medicine was absorbed in your gut. You don’t need to take another dose.
What should I do if I accidentally crush or split my extended-release pill?
Call your pharmacist or doctor right away. Don’t wait for symptoms. If it’s a high-risk drug like an opioid, ADHD medication, or heart medicine, you may need to be monitored. Keep the empty shell or packaging - it helps them understand what you took. In the future, always ask for a different form if swallowing is hard.
Why do some extended-release labels say "24 hour" and others don’t?
FDA guidelines now require the duration (like "24 hour" or "12 hour") to be clearly stated on the label. Older labels might not have it. If you’re unsure how long your pill lasts, ask your pharmacist. Never assume - a 12-hour pill taken once a day won’t work right. The duration is part of the safety design.
Next Steps: What to Do Today
If you’re taking an extended-release medication:- Look at your label. Find the ER, XR, SR, or CR.
- Read the “Directions.” Note the time of day and whether it’s with or without food.
- Check for “DO NOT CRUSH, SPLIT, OR CHEW.” If it’s there, remember it.
- Ask your pharmacist: “Is this the same as my last bottle?” If the brand changed, it might be a different release system.
- Set a phone reminder. Don’t rely on memory. These pills are designed for consistency.
Medication safety isn’t about being perfect. It’s about being careful. One small mistake - crushing a pill, taking it at the wrong time - can undo years of treatment. But one small step - reading the label - can save your life.
9 Comments
Write a comment
More Articles

Shortage mitigation strategies: what health systems are doing to fight workforce gaps
Health systems are tackling workforce shortages with flexible scheduling, AI tools, cross-training, and community partnerships. Learn what’s actually working to keep hospitals running and staff from burning out.
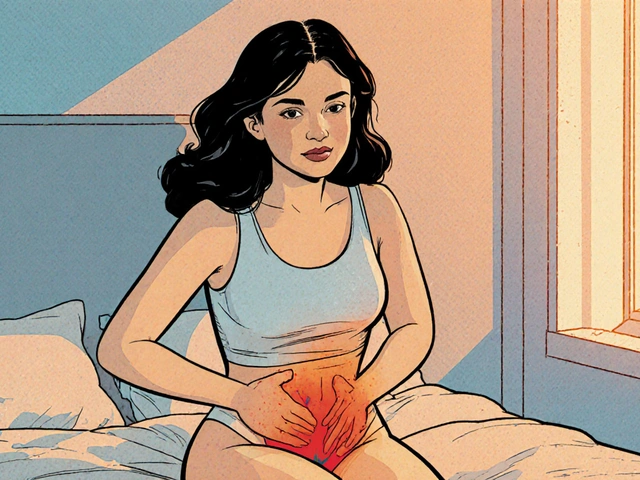
Understanding Vaginal Burning and Its Connection to Chronic Pelvic Pain
Explore how vaginal burning can signal chronic pelvic pain, its causes, diagnosis, and practical treatment steps for lasting relief.
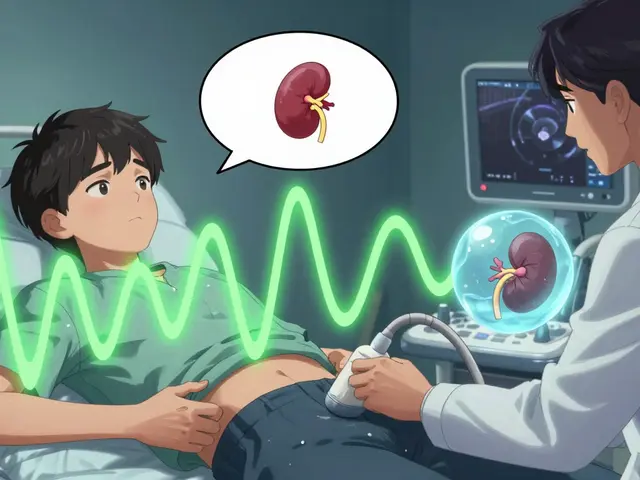
Renal Ultrasound and Imaging: Evaluating Obstruction and Size
Renal ultrasound is the safest, most widely used first-line tool for evaluating kidney obstruction and size. It detects hydronephrosis, measures kidney length and blood flow, and avoids radiation - making it ideal for kids, pregnant patients, and repeat monitoring.
Bryan Coleman
February 1, 2026 AT 16:14Just took my dad to the pharmacy yesterday and he asked why his blood pressure pill says 'do not crush' - I had no idea. This post saved us both from a potential disaster. Thanks for laying it out so clearly.