Antifungal Resistance: Why Common Treatments Are Failing and What You Can Do
When you think of drug resistance, you probably think of antibiotics and superbugs. But antifungal resistance, the ability of fungi to survive treatments meant to kill them. Also known as fungal drug resistance, it’s quietly becoming a global health threat—just like antibiotic resistance, but with fewer treatment options. Fungi like Candida albicans, a common yeast that causes thrush and vaginal infections and Aspergillus fumigatus, a mold that can cause deadly lung infections are evolving faster than our drugs can keep up. Hospitals are seeing more cases where standard antifungal drugs like fluconazole or echinocandins simply don’t work anymore.
This isn’t just a hospital problem. Overuse of antifungals in agriculture, unnecessary antifungal creams for minor skin rashes, and long-term use of antifungal pills for chronic infections are all feeding this crisis. People with weakened immune systems—those on chemotherapy, organ transplants, or long-term steroids—are most at risk. But even healthy people are starting to see stubborn infections that won’t clear up, no matter how many times they reapply the cream or refill the prescription. The antifungal drugs, medications designed to kill or stop the growth of fungi we’ve relied on for decades are losing their edge. And unlike antibiotics, we don’t have a long pipeline of new antifungals coming out. The ones we do have are often toxic, expensive, or hard to administer.
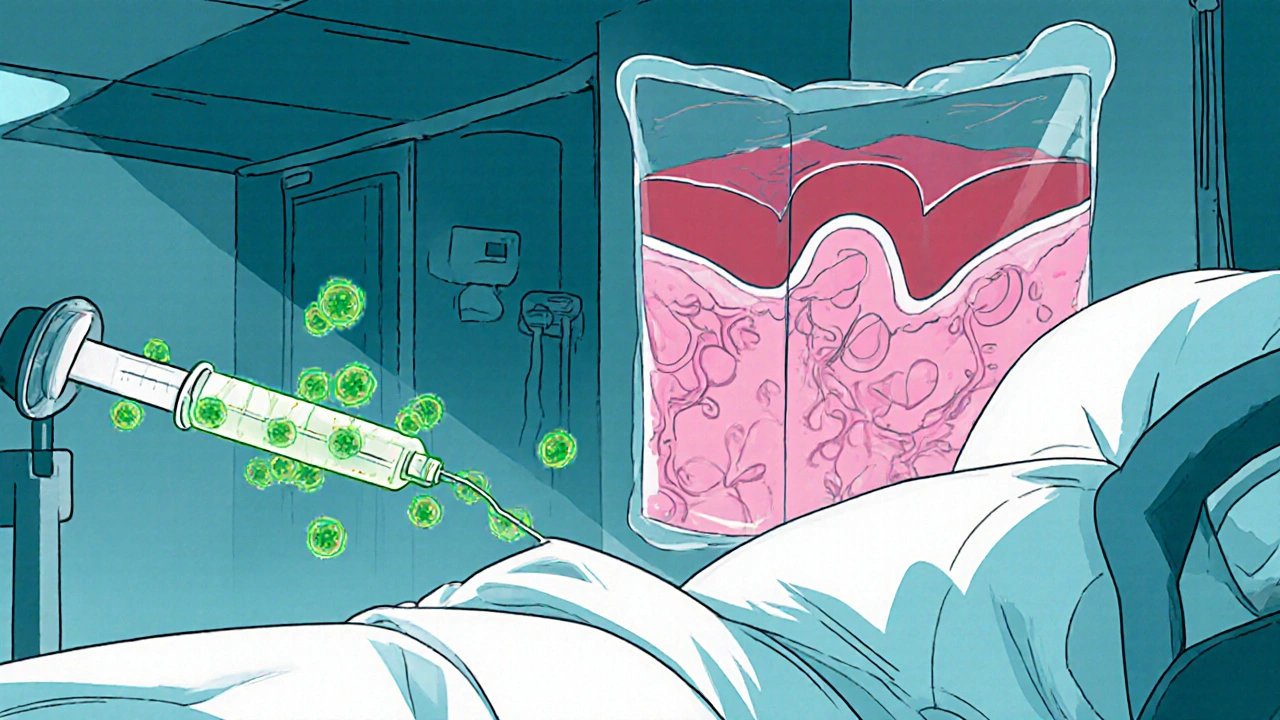
What’s worse? Many of these resistant fungi spread silently. You might not know you’re carrying one until it causes a serious infection. And once it does, treatment becomes a gamble—switching drugs, increasing doses, or combining medications with unpredictable results. Some cases now require weeks of IV antifungals, hospital stays, or even surgery. The good news? Awareness is growing. Doctors are starting to test for resistance before prescribing. Researchers are exploring new drug classes and even non-drug approaches like probiotics and phage therapy. Meanwhile, you can help by only using antifungals when truly needed, finishing your full course, and avoiding OTC creams for undiagnosed rashes.
Below, you’ll find real-world guides on how antifungal resistance affects everyday treatments—from the antibiotics you might be taking that weaken your defenses, to how certain medications like corticosteroids can make fungal infections worse. You’ll also see how doctors assess drug reactions, when to question a prescription, and how to spot when a "simple" infection is becoming something more dangerous. This isn’t theoretical. These are the stories behind the rising numbers. Know what you’re up against. Know what to ask. And know when to push back.
Rising Threat of Candidemia and Disseminated Candida Infections in Hospitals
Explore why candidemia and disseminated Candida infections are rising in hospitals, learn to identify at‑risk patients, diagnose quickly, treat effectively, and prevent outbreaks with proven strategies.