Compounded Medications: What They Are, When They're Used, and What You Need to Know
When a regular pill or capsule won’t work for you, compounded medications, custom-made drug formulations prepared by specialized pharmacies to meet individual patient needs. Also known as custom prescriptions, they’re mixed from scratch using raw ingredients to match a doctor’s exact instructions. This isn’t just about flavoring medicine for kids—it’s often the only way someone can get the right dose, avoid an allergen, or get a drug that’s been pulled from the market.
Compounding pharmacies, licensed facilities that prepare personalized medications outside standard manufacturing processes. Also known as pharmacy compounding, these aren’t big drugmakers—they’re local labs staffed by pharmacists who mix, crush, or blend drugs by hand. You’ll find them making things like hormone creams for menopause, pain patches without alcohol, or liquid versions of pills for people who can’t swallow. Some even make sterile compounding, the preparation of injectable or IV medications under strict clean-room conditions for cancer patients or hospital use. These aren’t just convenience options—they’re lifelines for people with rare conditions or severe allergies.
But here’s the catch: because these aren’t mass-produced, they don’t go through the same FDA testing as regular drugs. That means quality can vary. Some compounding pharmacies follow strict guidelines. Others cut corners. You need to know where your meds come from. Look for pharmacies accredited by the PCAB or licensed by your state board. Ask if they test their batches. If you’re getting something like a hormone cream or a pain gel, make sure it’s made in a clean environment—especially if it’s going into your bloodstream.
People turn to compounded meds for all kinds of reasons: maybe they’re allergic to dye in standard pills, or their child refuses to take a bitter liquid, or their doctor needs a dose that doesn’t exist commercially. Some use them for thyroid treatment, hormone replacement, or even to stop taking a drug that’s been discontinued. The posts below show real cases—like how patients manage side effects from custom hormone blends, how sterile compounding affects hospital outcomes, and why some doctors avoid these formulas unless absolutely necessary. You’ll find practical advice on asking the right questions, spotting red flags, and working with your pharmacist to get safe, effective results.
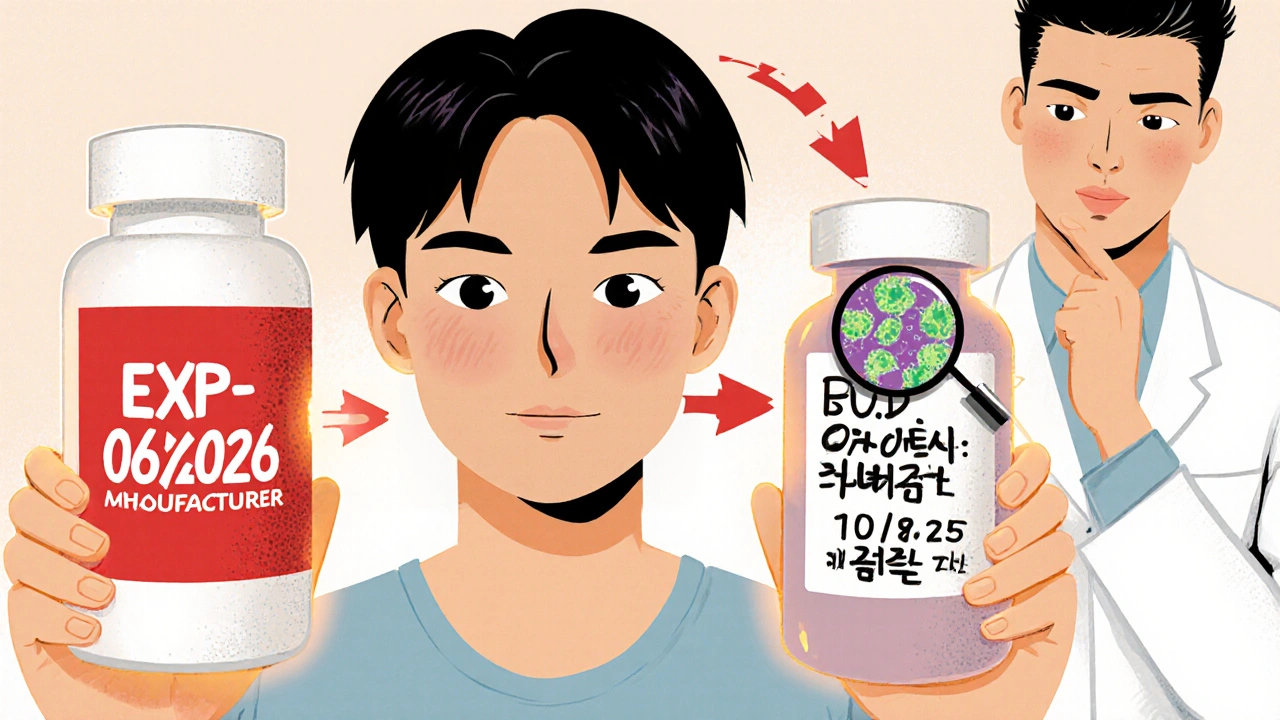
How to Compare Manufacturer Expiration Dates vs. Pharmacy Beyond-Use Dates
Learn the critical difference between manufacturer expiration dates and pharmacy beyond-use dates for compounded medications. Know when your medicine is safe to use-and when to throw it away.