Disseminated Candida Infection – What It Is and How to Manage It
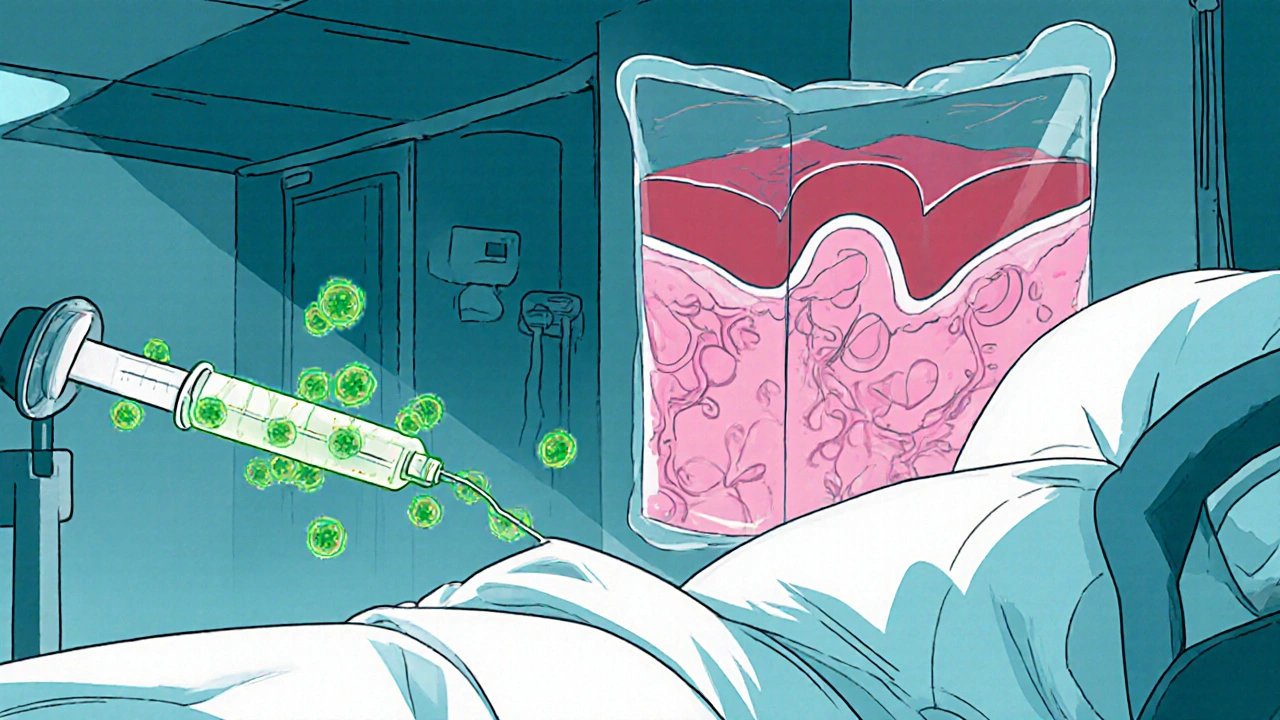
When dealing with disseminated candida infection, a severe, blood‑borne fungal invasion that spreads to multiple organs. Also known as systemic candidiasis, it usually strikes people whose immune systems are weakened or whose medical devices provide a portal for fungi. Understanding the infection’s biology, the patients most at risk, and the tools doctors use to fight it can make the difference between a quick recovery and a life‑threatening crisis.
One of the biggest drivers of immunosuppression, conditions or treatments that blunt the body’s natural defenses is the use of chemotherapy, high‑dose steroids, or organ‑transplant medications. Those same therapies often appear in our other articles, such as the discussion about hydroxyurea’s impact on bone health or the Naranjo Scale for drug reaction assessment. When the immune system can’t keep Candida in check, the fungus can slip from the gut or skin into the bloodstream, traveling to the kidneys, eyes, brain, and heart. This chain of events shows why a solid grasp of disseminated candida infection requires linking risk factors, diagnostic steps, and treatment choices.
How Doctors Spot a Systemic Fungal Threat
Diagnosis hinges on a few key actions. First, clinicians draw blood cultures to catch the yeast as it circulates – a direct confirmation that the infection is not just localized. Imaging studies, like CT or MRI, help locate hidden organ involvement, while lab markers such as beta‑D‑glucan can raise suspicion early. In articles about head‑ache types or eye‑drop comparisons, we see similar reliance on targeted tests to pinpoint the problem. The diagnostic pipeline for disseminated candida infection illustrates the semantic triple: disseminated candida infection requires accurate blood cultures, and those cultures guide effective antifungal therapy.
Once the pathogen is identified, the treatment plan kicks in. The cornerstone is antifungal therapy, medicines like echinocandins, fluconazole, or amphotericin B that directly attack Candida cells. Choice of drug depends on the species, patient kidney function, and severity of organ involvement. For instance, an echinocandin may be started right away in a critically ill patient, then switched to oral fluconazole once stability returns. This mirrors the step‑by‑step approach we champion in guides about compression stockings or generic medication purchases – start with the most potent option, then transition to a maintenance phase.
Beyond drugs, supportive care matters. Managing central lines, controlling blood glucose, and reducing steroid doses where possible all shrink the fungus’s foothold. Our piece on hydroxyurea and bone health highlighted how adjusting accompanying treatments can limit side effects; the same principle applies here – tweak the surrounding medical environment to boost the antifungal’s impact. Together, these strategies form another semantic triple: effective antifungal therapy reduces mortality, and adjunctive measures enhance drug efficacy.
Armed with this overview, you’ll recognize the patterns that tie together risk, detection, and cure across many of our articles. Below you’ll find a curated list of posts that dive deeper into related drugs, side‑effect management, and infection‑control tactics – all valuable pieces for anyone facing or studying disseminated candida infection.
Rising Threat of Candidemia and Disseminated Candida Infections in Hospitals
Explore why candidemia and disseminated Candida infections are rising in hospitals, learn to identify at‑risk patients, diagnose quickly, treat effectively, and prevent outbreaks with proven strategies.