Infection Control: Your Guide to Staying Safe
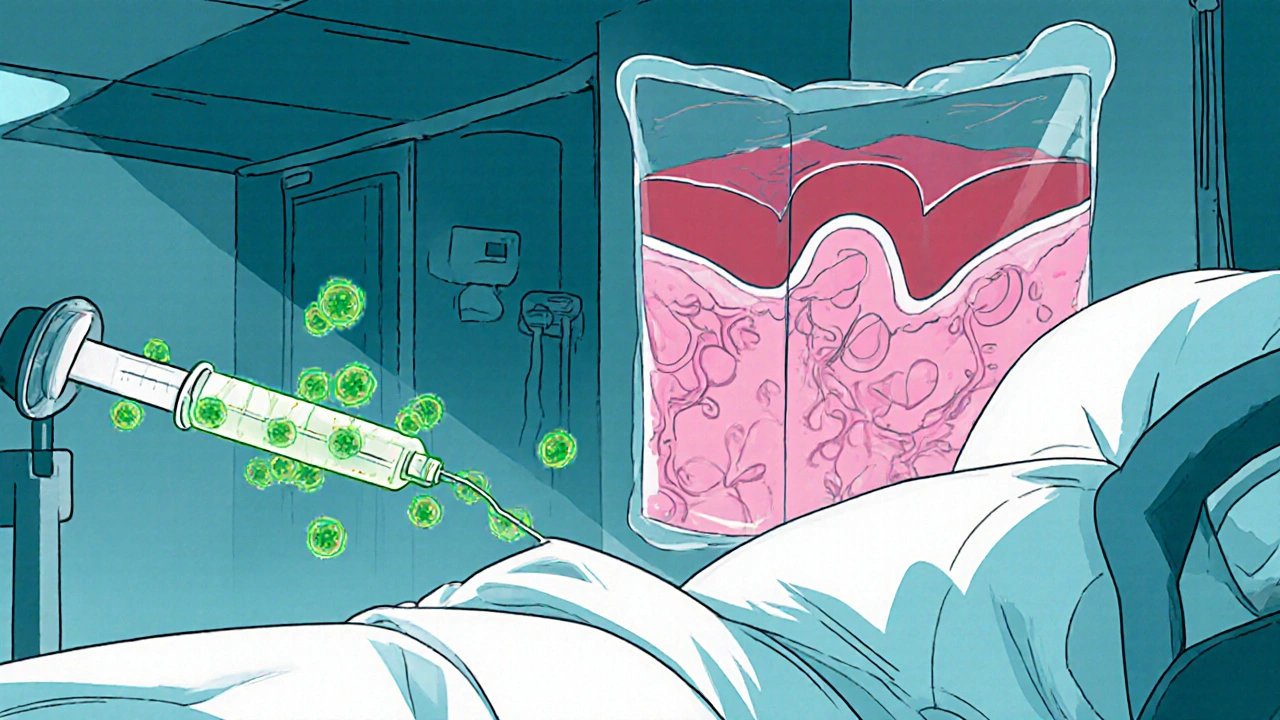
When talking about Infection Control, the set of practices that prevent the spread of harmful germs in healthcare and community settings. Also known as infection prevention, it covers everything from cleaning surfaces to training staff on safety measures.
infection control isn’t a buzzword; it’s a daily routine that saves lives. Think of it as a shield that stops microbes before they cause trouble. The backbone of that shield is hand hygiene, the simple act of washing or sanitizing hands at key moments. Hand hygiene encompasses the use of soap, water, and alcohol‑based rubs, and it’s the single most effective way to cut transmission rates. When you wash your hands properly, you’re actively reducing the pathogen load on your skin, which directly limits the chance of spreading infections.
Another pillar is personal protective equipment, gear like masks, gloves, gowns, and eye shields that create a barrier between you and infectious agents. Effective infection control requires proper PPE, because the gear blocks droplets and contact that would otherwise bypass hand hygiene. Choosing the right mask for a flu season or wearing gloves during a wound dressing are practical ways the equipment protects both patients and caregivers.
Cleaning and sterilizing the environment falls under sterilization, the process of eliminating all viable microorganisms from surfaces, instruments, or air. This goes beyond a quick wipe – it involves validated disinfectants, UV light, or autoclave cycles for equipment that enters the body. When hospitals follow strict sterilization protocols, they dramatically lower the risk of surgical site infections and other hospital‑acquired problems.
Beyond the physical barriers, antimicrobial stewardship, the coordinated effort to use antibiotics responsibly and curb resistance, influences infection control outcomes. By prescribing the right drug, dose, and duration, clinicians prevent the emergence of superbugs that can outsmart standard cleaning and hand‑washing measures. Good stewardship means fewer resistant infections, which in turn eases the burden on hygiene and sterilization teams.
All these pieces – hand hygiene, PPE, sterilization, and stewardship – come together during an outbreak. Managing a sudden rise in cases, whether it’s a flu surge or a hospital‑borne outbreak, requires coordinated response plans, rapid testing, and clear communication. When each element works in sync, the spread slows, and patients stay safer. This integrated approach shows how infection control encompasses multiple linked actions.
Below you’ll find a hand‑picked collection of articles that dive deeper into each of these topics. From practical guides on proper hand‑washing technique to the latest on antimicrobial stewardship, the posts are packed with tips you can start using right away. Keep reading to boost your knowledge and protect the people around you.
Rising Threat of Candidemia and Disseminated Candida Infections in Hospitals
Explore why candidemia and disseminated Candida infections are rising in hospitals, learn to identify at‑risk patients, diagnose quickly, treat effectively, and prevent outbreaks with proven strategies.