Paroxetine Dosage: Finding the Right Amount
When working with paroxetine dosage, the prescribed amount of the SSRI paroxetine used to treat mood and anxiety disorders. Also known as Paxil dose, it determines how well the drug balances serotonin while keeping side effects in check.
Paroxetine dosage isn’t a one‑size‑fits‑all number. It starts low—usually 10 mg per day for adults—then climbs based on how the patient feels. This step‑up approach follows the principle that starting low and going slow reduces adverse reactions and improves adherence. In practice, clinicians watch for therapeutic response, then may increase to 20 mg or 40 mg if needed.
Key Factors That Shape Your Dose
One major factor is the drug class itself. Selective serotonin reuptake inhibitor a group of antidepressants that boost serotonin levels in the brain includes paroxetine, fluoxetine, sertraline, and others. Because SSRIs share a similar mechanism, they also share dosing patterns and side‑effect profiles. Understanding that paroxetine has a relatively short half‑life (about 21 hours) helps doctors decide whether a once‑daily or split dose works best for a specific metabolism.
Another central entity is the condition being treated. Depression a mood disorder marked by persistent sadness, loss of interest, and fatigue often requires a higher maintenance dose to sustain mood elevation, while Generalized anxiety disorder excessive worry and tension without a clear trigger may respond to lower doses that still calm the nervous system. This link between condition and dosage is a classic semantic triple: Paroxetine dosage guidelines encompass condition‑specific targets.
Patient age and liver function also matter. Elderly patients metabolize paroxetine more slowly, so starting at 10 mg and staying there longer is common. Liver impairment can raise blood levels, increasing the risk of nausea, dizziness, or sexual dysfunction. When side effects appear, the dosage may be reduced or a slower titration schedule adopted. Here’s another triple: Effective dosage requires matching drug half‑life with patient metabolism.
Drug interactions play a big role, too. Combining paroxetine with other serotonergic agents (like tramadol or triptans) can trigger serotonin syndrome, a potentially life‑threatening condition. Clinicians therefore check for concomitant medications before adjusting the dose. This creates a semantic link: Paroxetine dosage influences and is influenced by other serotonergic drugs.
Gender differences are subtle but worth noting. Women sometimes experience stronger side effects at equivalent doses, possibly due to hormonal influences on serotonin pathways. Adjustments based on gender can improve tolerability without sacrificing efficacy.
Lastly, patient adherence impacts the real‑world dose. Missing doses or stopping abruptly can lead to withdrawal symptoms—often described as “brain zaps.” To avoid this, doctors may recommend tapering schedules when lowering the dose, turning the dosage plan into a gradual curve rather than a sharp drop.
All these elements—drug class, condition, age, liver health, interactions, gender, and adherence—form a network of factors that guide clinicians toward the optimal paroxetine dosage for each individual. Below you’ll find a curated set of articles that break down dosage calculations, safety tips, and how paroxetine interacts with other medicines, giving you practical tools to manage your treatment confidently.
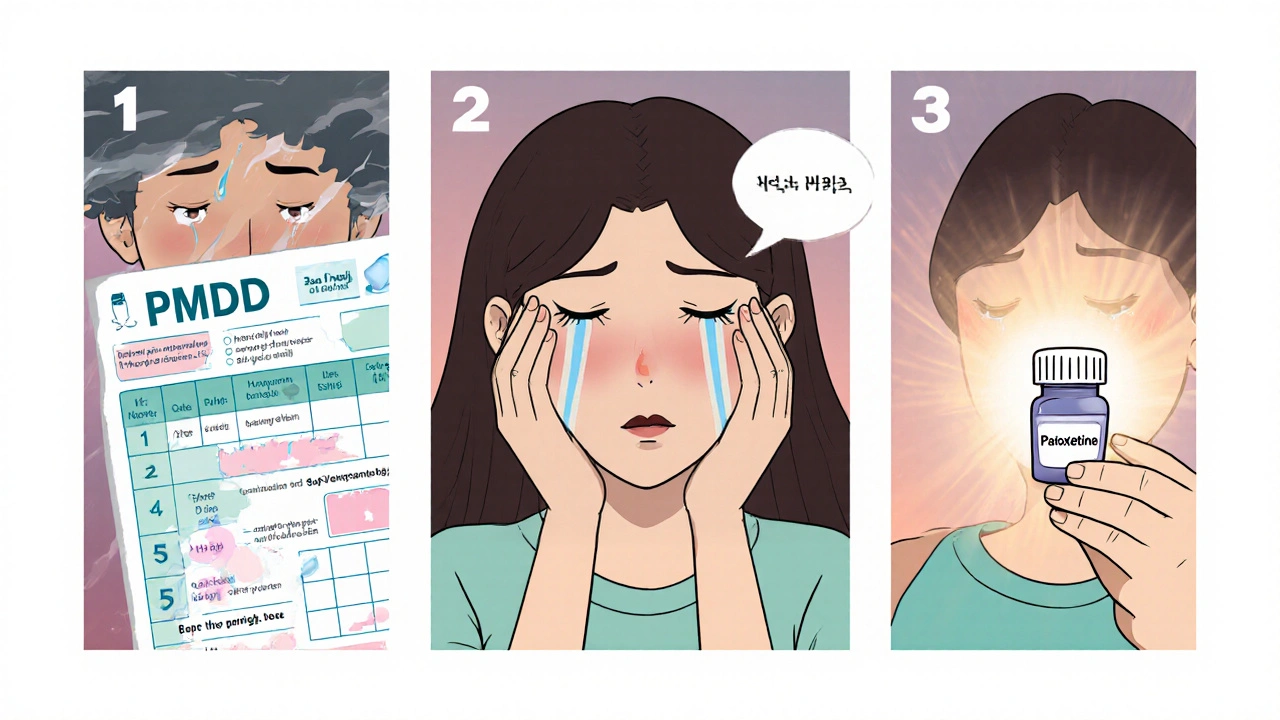
How Paroxetine Can Help Treat Premenstrual Dysphoric Disorder
Learn how paroxetine, an FDA‑approved SSRI, treats Premenstrual Dysphoric Disorder, including dosage, effectiveness, side‑effects, and comparisons with other therapies.