Pelvic Pain Causes: Understanding What Triggers Discomfort
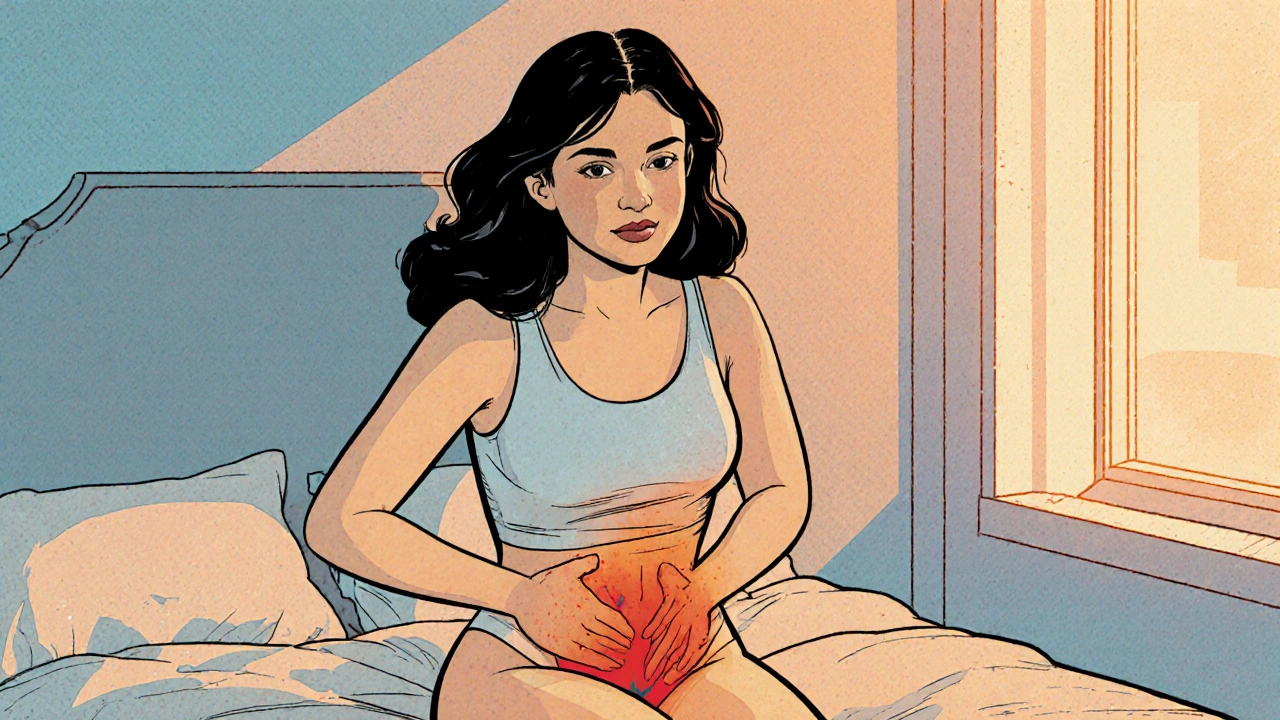
When dealing with pelvic pain, a deep ache or pressure felt in the lower abdomen and surrounding areas. Also known as lower abdominal discomfort, it can stem from many different health issues. Knowing the root helps you choose the right plan, whether it’s a simple lifestyle tweak or a doctor’s visit.
One major endometriosis, tissue similar to the uterine lining that grows outside the uterus. E can cause cyclical cramps, painful periods, and chronic pelvic ache. Another frequent offender is urinary tract infection, bacterial inflammation of any part of the urinary system. It often starts with a burning sensation when you pee, then spreads to a dull ache in the pelvis. pelvic pain causes also include musculoskeletal strain, tight or injured muscles, ligaments, and joints in the lower back and hips. Even everyday activities like lifting heavy bags or long bike rides can trigger that deep throb. Lastly, irritable bowel syndrome, a functional gut disorder that causes bloating, gas, and irregular bowel movements, often sends pain radiating to the pelvic region.
Common Triggers to Watch
Pelvic pain encompasses gynecological, urological, musculoskeletal, and gastrointestinal sources. It requires a systematic look at symptoms, timing, and lifestyle clues. For example, pain that worsens during menstruation usually points to a gynecologic issue like endometriosis or ovarian cysts. Pain that spikes after drinking coffee or after a large meal may hint at gut irritation or IBS. If you notice soreness after a workout, think muscle strain or pelvic floor dysfunction.
Each cause brings its own set of red flags. Endometriosis often produces deep, stabbing cramps that don’t ease with over‑the‑counter painkillers. UTIs present with frequent urination, cloudy urine, and sometimes fever. Musculoskeletal strain shows up as localized tenderness that improves with gentle stretching or heat. IBS‑related pain tends to be crampy, moves around, and is accompanied by changes in stool consistency.
Understanding these patterns lets you talk to your healthcare provider with clear details. It also guides you toward self‑care steps that can reduce flare‑ups: staying hydrated to flush bacteria, using heat packs for muscle tightness, tracking your cycle to spot hormonal links, and following a low‑FODMAP diet if gut symptoms dominate.
Below you’ll find a curated list of articles that dig deeper into each of these areas. From practical dosage guides for meds that manage pain to lifestyle hacks that support pelvic health, the collection gives you actionable insight no matter where your discomfort originates. Ready to explore the specifics? Let’s get into the details.
Understanding Vaginal Burning and Its Connection to Chronic Pelvic Pain
Explore how vaginal burning can signal chronic pelvic pain, its causes, diagnosis, and practical treatment steps for lasting relief.