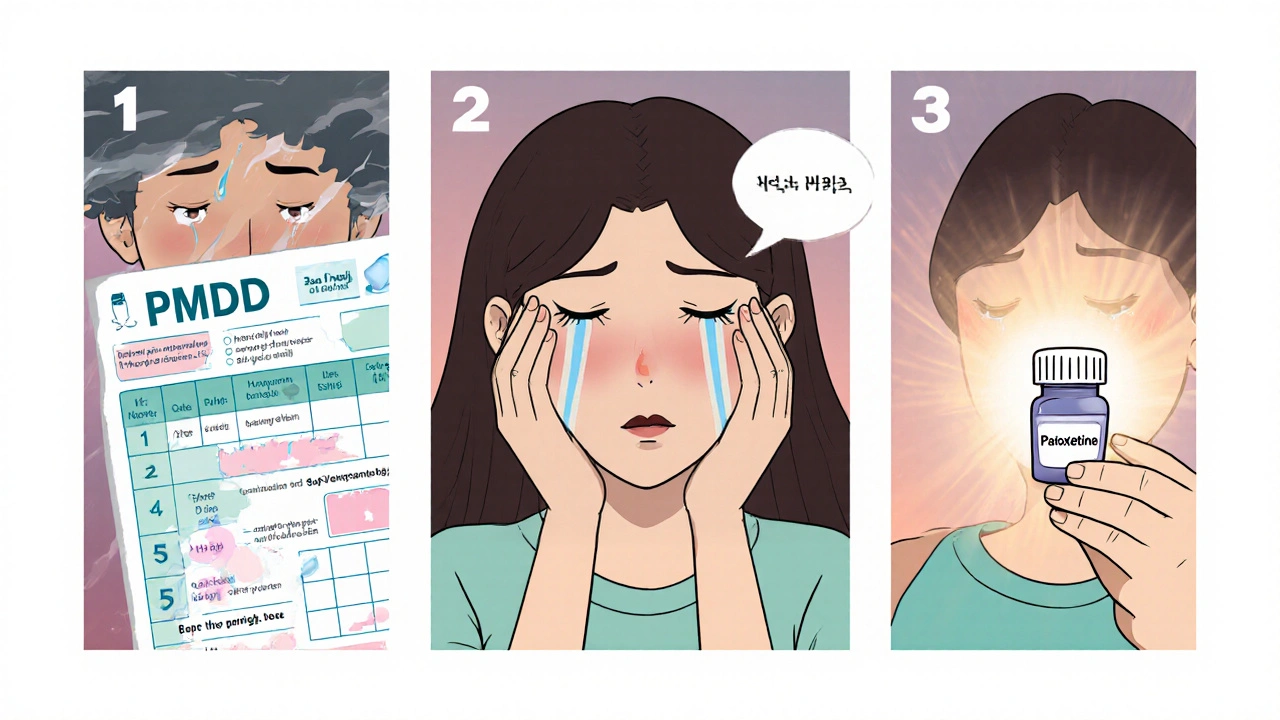
PMDD Treatment: What Works and Why
When talking about PMDD treatment, the medical and therapeutic steps used to lessen severe premenstrual symptoms. Also known as premenstrual dysphoric disorder therapy, it focuses on reducing mood swings, physical pain, and functional impairment that many women face each month. PMDD treatment is not a one‑size‑fits‑all solution; it blends drugs, hormone management, counseling, and daily habits to target the disorder from several angles.
Key Approaches to Managing PMDD
One of the most common medical routes is the use of SSRIs, selective serotonin reuptake inhibitors that boost serotonin levels and stabilize mood. These pills can be taken continuously or only during the luteal phase, and they often start working within a few days. Another pillar is hormonal therapy, treatments that adjust estrogen and progesterone fluctuations, such as oral contraceptives or GnRH agonists. Hormonal tweaks address the root hormonal swing that triggers PMDD symptoms, making the mood and physical complaints less intense. Beyond medication, many find CBT, cognitive‑behavioral therapy that teaches coping skills and thought pattern changes invaluable. CBT helps break the cycle of negative thinking that often worsens mood swings, and it equips patients with strategies for stress management. Lifestyle changes also play a huge role: regular exercise, a balanced low‑salt diet, adequate sleep, and limiting caffeine and alcohol can all blunt symptom spikes. The triplet of medication, therapy, and lifestyle creates a comprehensive plan where each piece supports the others.
Clinical practice shows that successful PMDD treatment requires an individualized mix. A patient might start with an SSRI, add a low‑dose oral contraceptive, and begin weekly CBT sessions while tracking triggers in a symptom diary. That diary feeds back into the treatment loop, letting doctors fine‑tune dosages or swap approaches when needed. The synergy between hormonal regulation and mental‑health techniques often yields the best outcomes, and it illustrates how effective PMDD treatment requires both pharmacologic and psychosocial components. Below you’ll find articles that cover each of these angles in depth – from detailed drug dosing guides to practical tips for managing stress during the luteal phase. Dive into the collection to see real‑world advice, research updates, and step‑by‑step recommendations that can help you build a tailored PMDD management plan.
How Paroxetine Can Help Treat Premenstrual Dysphoric Disorder
Learn how paroxetine, an FDA‑approved SSRI, treats Premenstrual Dysphoric Disorder, including dosage, effectiveness, side‑effects, and comparisons with other therapies.