Rural Patients: Challenges, Medication Access, and Solutions
When we talk about rural patients, people living in remote or underserved areas who struggle to access consistent medical care and medications. Also known as frontier patients, they often live miles from the nearest pharmacy, clinic, or specialist. This isn’t just about distance—it’s about systems that weren’t built for them. While urban areas get new drugs, telehealth tools, and same-day prescriptions, rural patients are left waiting weeks for a refill, driving hours to see a doctor, or skipping doses because they can’t afford the trip.
One major issue is pharmacy shortages, the lack of local pharmacies in rural counties, forcing patients to rely on mail-order or distant providers. Over 60% of rural counties in the U.S. have no pharmacy at all. That means if your blood pressure med runs out, you can’t just walk in and get a new bottle. You might need to call ahead, wait for a shipment, or risk going without. And it’s not just pills—insulin, inhalers, anticoagulants, and even basic pain relievers become logistical nightmares. Add to that healthcare disparities, systemic gaps in care quality, provider availability, and insurance coverage between urban and rural populations, and you’ve got a situation where people with chronic conditions like diabetes, asthma, or heart disease are far more likely to end up in the ER because their meds ran out or their symptoms weren’t managed early enough.
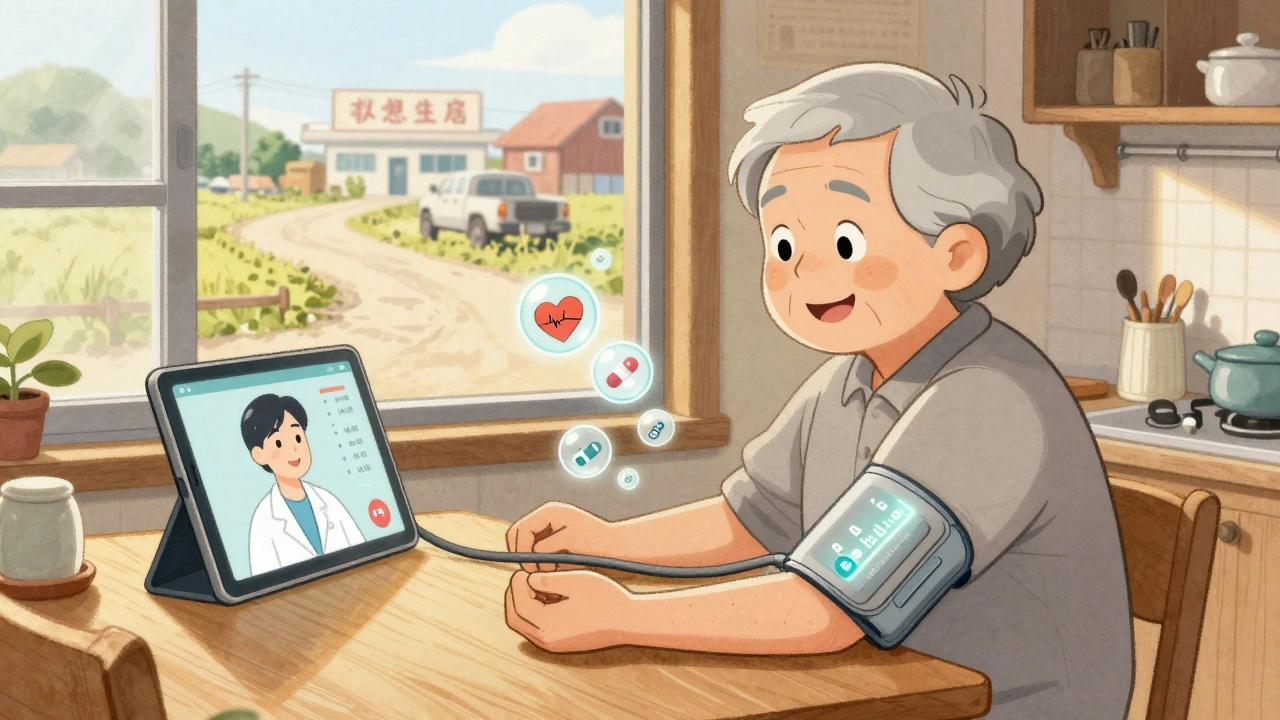
But it’s not all bleak. Many rural clinics are now using telehealth for rural communities, virtual visits that connect patients with pharmacists, specialists, and care coordinators without requiring travel. Some pharmacies partner with local churches, schools, or community centers to offer drop-off points for prescriptions. Others use mobile vans that rotate through towns on a schedule. These aren’t perfect fixes, but they’re real steps forward. And the posts below show exactly how these solutions play out in practice—from managing anticoagulants in remote areas to dealing with generic pill changes when you don’t have a pharmacist nearby to explain them.
What you’ll find here aren’t abstract theories. These are real stories from rural clinics, patient experiences with medication delays, how poison control hotlines get used differently when you’re 40 miles from a hospital, and how people are adapting when the nearest specialist is a two-hour drive away. If you’re a rural patient, a caregiver, or just someone who wants to understand what life looks like when healthcare feels out of reach—this is the guide you need.
Telehealth Strategies for Monitoring Side Effects in Rural and Remote Patients
Telehealth is transforming how rural and remote patients manage medication side effects. From smart devices to pharmacist-led monitoring, discover how these strategies reduce hospitalizations and save lives in underserved areas.