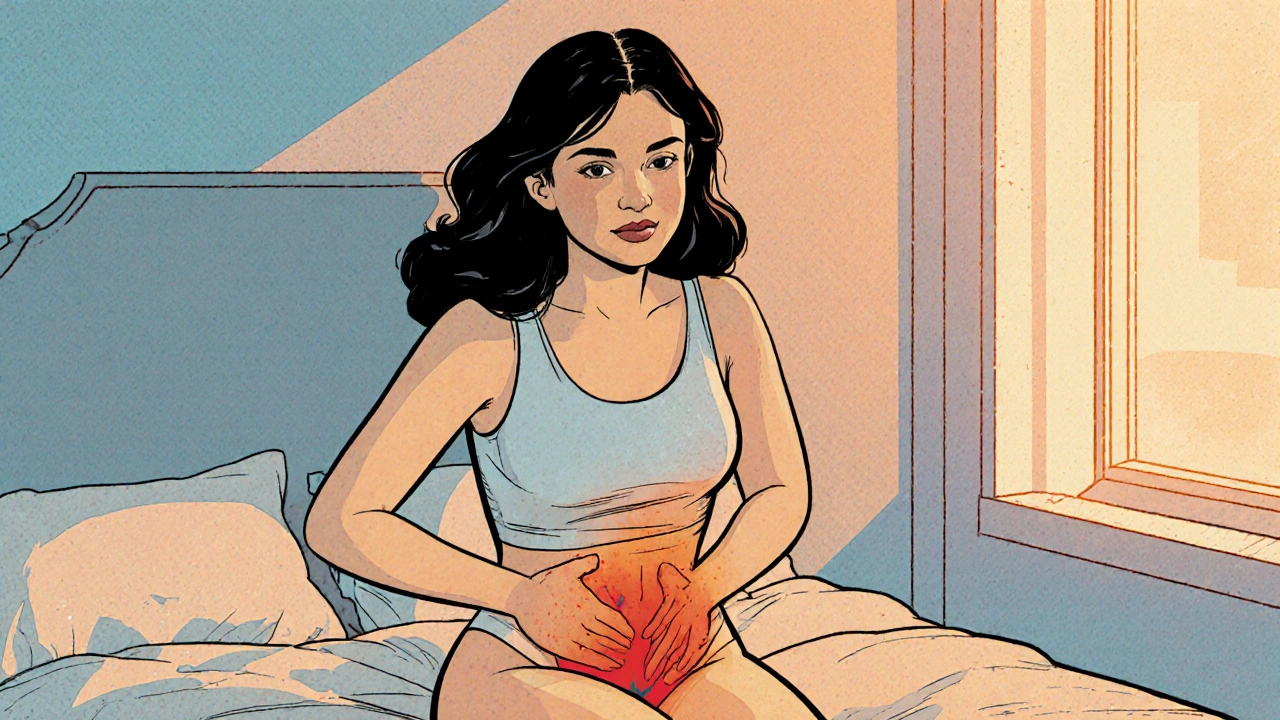
Vulvodynia: Understanding the Condition
When talking about vulvodynia, persistent pain or discomfort in the vulvar area without an obvious cause. Also known as vulvar pain syndrome, it affects many women at different ages and can linger for months or years. Vulvodynia isn’t just a fleeting irritation; it’s a chronic condition that can interfere with intimacy, exercise, even simple sitting. Research shows that up to 16% of women experience some form of vulvar pain, but only a fraction get an accurate diagnosis. The condition often overlaps with pelvic floor dysfunction, where the muscles around the pelvis become overly tight or weak, amplifying discomfort. Hormonal shifts, especially during menopause or after childbirth, are another frequent trigger, linking hormonal changes directly to the pain cycle. In short, vulvodynia sits at the crossroads of neurology, gynecology, and musculoskeletal health, demanding a holistic view.
Key Factors and Treatment Pathways
Typical symptoms range from burning and stinging to sharp, itching sensations, all of which worsen with activities like intercourse, cycling, or prolonged sitting. Because the pain can mimic infections, many women first receive antibiotics for suspected bacterial vaginosis or yeast overgrowth, only to find relief short‑lived. Accurate diagnosis usually involves a detailed history, a pelvic exam, and sometimes a “cotton swab test” to pinpoint tender spots. Once ruled out, clinicians often turn to chronic pain management strategies: topical anesthetics, oral neuropathic agents, and low‑dose tricyclic antidepressants are common first‑line meds. Physical therapy focused on the pelvic floor can release muscle tension, while cognitive‑behavioral therapy helps reframe the pain experience. Emerging evidence also highlights the role of diet, vitamin D levels, and even mindfulness‑based stress reduction in easing symptoms. Each of these avenues reflects a semantic triple: vulvodynia requires multidisciplinary care; pelvic floor therapy reduces muscle‑related pain; hormonal changes can exacerbate nerve sensitivity.
Putting all this together, the road to relief often means mixing medication, therapy, and lifestyle tweaks. Below you’ll find a curated set of articles that dive deeper into each option—whether you need a practical guide on medication dosing, tips for effective pelvic floor exercises, or advice on navigating sexual intimacy while coping with vulvar pain. These resources aim to empower you with clear steps, real‑world examples, and up‑to‑date research, so you can move from frustration to a manageable, healthier everyday life.
Understanding Vaginal Burning and Its Connection to Chronic Pelvic Pain
Explore how vaginal burning can signal chronic pelvic pain, its causes, diagnosis, and practical treatment steps for lasting relief.