
For over a billion people worldwide, migraine isn’t just a bad headache. It’s a neurological event that can knock you out for hours-or days. The pain is often one-sided, throbbing, and so intense that light or sound becomes unbearable. Nausea rolls in. You cancel plans. You lie in a dark room. And if this happens 15 or more days a month, you’re not dealing with occasional migraines-you’re living with chronic migraine disorder.
What Makes Migraine Different From a Regular Headache?
Migraine isn’t caused by stress or dehydration alone. It’s a genetic neurological condition, recognized since the 1980s by the International Headache Society. The current diagnostic standard, ICHD-3, says a migraine attack without aura must last 4 to 72 hours, involve pulsating pain, be made worse by movement, and come with nausea, sensitivity to light, or sensitivity to sound. About 30% of people with migraine also experience aura-a visual disturbance like flashing lights or blind spots, or sometimes numbness or speech trouble-that starts slowly and lasts 5 to 60 minutes before the headache hits.
Most people don’t need an MRI or CT scan to be diagnosed. A neurologist who knows the criteria can spot it with 95% accuracy just by asking the right questions. But too many people are misdiagnosed with sinus headaches or tension headaches, especially in primary care. That’s why tracking your symptoms matters.
Preventive Treatments: Stopping Migraines Before They Start
If you’re having more than four migraine days a month, prevention should be part of your plan. There are two kinds: medications and non-drug approaches.
Traditional preventive meds include beta-blockers like propranolol, antiseizure drugs like topiramate, and calcium channel blockers like verapamil. These have been around for decades and work for about half the people who try them. But side effects are common: topiramate can make you forget words, feel foggy, or lose your appetite. Beta-blockers might cause fatigue or low blood pressure.
Then came the breakthrough: CGRP monoclonal antibodies. These are the first migraine-specific preventives. Drugs like erenumab (Aimovig), fremanezumab (Ajovy), and galcanezumab (Emgality) block a protein in the brain that triggers migraine. They’re injected monthly or quarterly. In clinical trials, 50-62% of users cut their migraine days by half or more. Side effects? Usually just mild injection-site reactions. The catch? They cost $650 to $750 a month. Insurance often denies them unless you’ve tried at least three older drugs first.
Botox is another option-but only for chronic migraine (15+ headache days a month). It’s given as 31 injections across the head and neck every 12 weeks. Studies show it cuts headache days by about 8 per month. Not a cure, but life-changing for many.
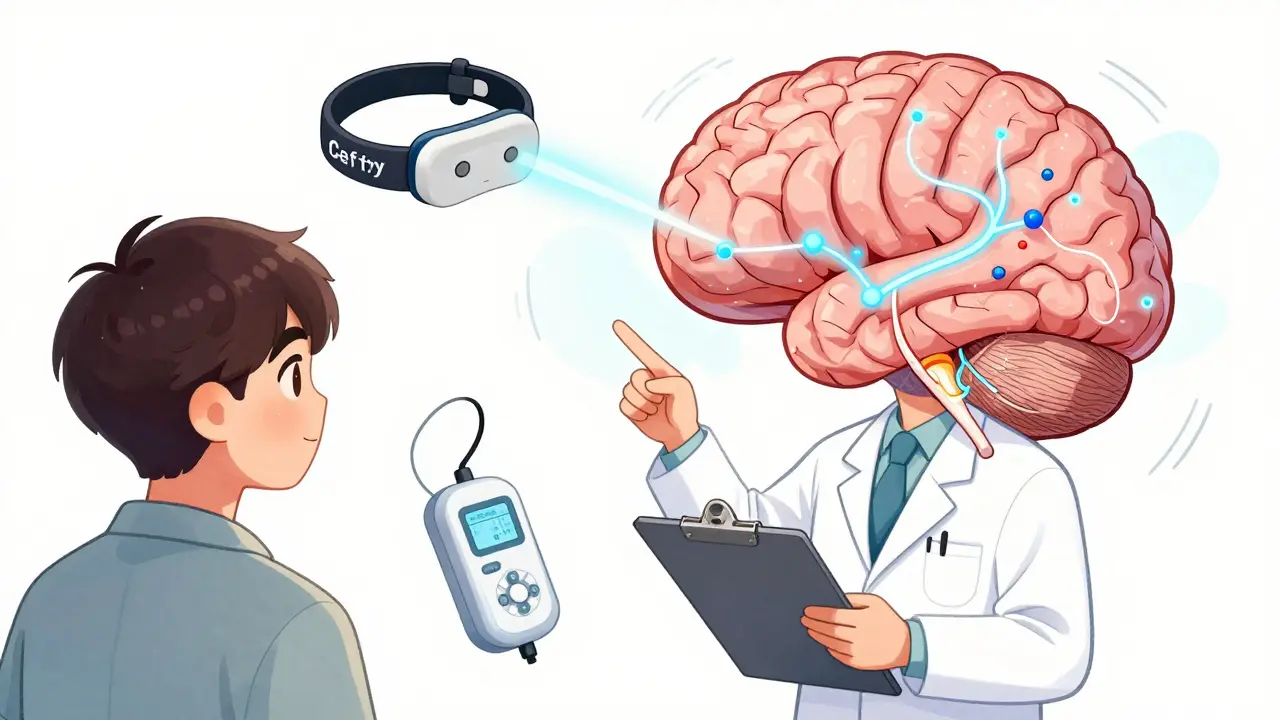
Non-drug options are growing fast. The Cefaly device is a headband you wear for 20 minutes a day. It sends gentle pulses to nerves above your eyebrows. In trials, 38% of users saw their migraine days drop by half. The gammaCore device stimulates the vagus nerve in your neck-used three times a day. Both are FDA-approved, medication-free, and safe for long-term use. Mindfulness and biofeedback also help. One 2022 study found an 8-week mindfulness program reduced headache frequency by 1.4 days per week.
Acute Treatment: Stopping a Migraine in Its Tracks
When a migraine hits, speed matters. The earlier you treat it, the better it works. Waiting until the pain is unbearable makes relief harder.
Over-the-counter painkillers like ibuprofen (400 mg) or naproxen (500 mg) can help mild attacks. Combination meds like Excedrin Migraine (aspirin + acetaminophen + caffeine) work for some-but using them more than 10 days a month can cause rebound headaches. That’s when your body gets dependent, and you start having headaches every day just to avoid withdrawal.
Triptans are the gold standard for moderate to severe attacks. Sumatriptan, rizatriptan, eletriptan-they come as pills, nasal sprays, or injections. They work by narrowing blood vessels in the brain and blocking pain signals. About 40% of people get completely pain-free within two hours. But they’re not safe for people with heart disease, high blood pressure, or a history of stroke. Side effects include chest tightness, dizziness, or a feeling of pressure.
Newer options are changing the game. Gepants like ubrogepant and rimegepant (Nurtec) block CGRP without affecting blood vessels. That means they’re safe for people who can’t take triptans. Rimegepant is also approved for prevention-making it the first drug you can use for both stopping an attack and preventing them. Ditans like lasmiditan work on brain receptors without narrowing blood vessels, so they’re safe for heart patients. But they can make you feel dizzy or sleepy.
For nausea, metoclopramide or prochlorperazine given as an injection can knock it out fast. These are common in ERs and work better than pills when you’re vomiting.
What Doesn’t Work-and What Can Make Things Worse
Opioids like oxycodone and barbiturates like butalbital should be avoided. They don’t treat migraine-they just mask it. And using them more than 10 days a month almost always leads to medication-overuse headache. That’s when your brain rewires itself to rely on the drug, and headaches become daily. Studies show 20-30% of people who overuse these meds end up with chronic migraine.
Also, don’t rely on caffeine alone. While a small amount in combination meds helps, drinking coffee or energy drinks daily can cause withdrawal headaches. Cutting back suddenly can trigger a migraine.
Real People, Real Results
One woman in Birmingham, 42, had 25 migraine days a month. She tried 12 medications. Nothing worked. Then she started using Cefaly daily. Within six months, her days dropped to nine. No side effects. No pills. She says it gave her life back.
Another man in his 50s couldn’t take triptans because of his heart condition. He started rimegepant. He went from 15 headache days a month to 4. He says, “I can finally play with my grandkids without dreading the next attack.”
But not everyone wins. One Reddit user wrote: “I used Excedrin 15 days a month. Got addicted. Ended up with daily headaches. Took six months to detox.” That’s medication-overuse headache in action.
Identifying Your Triggers
Triggers aren’t the cause of migraine-but they can set off an attack. The most common ones? Stress (89%), sleep changes (65%), weather shifts (72%), and certain foods (58%). Alcohol, aged cheese, MSG, and artificial sweeteners are frequent culprits. But here’s the thing: triggers vary wildly. What sets off one person’s migraine might do nothing for another.
Keeping a daily headache diary helps. Track what you ate, how much you slept, your stress level, and the weather. Apps like Headache Log make it easier than paper. People who track for 3-6 months start spotting patterns. One woman realized her migraines always came after her period-she now takes preventive meds during that window.

When to See a Specialist
You don’t need a specialist for occasional migraines. But if you’re having more than four days a month, if over-the-counter meds don’t help, or if you’re using acute treatments more than 10 days a month, see a headache specialist. Primary care doctors are getting better at this, but complex cases need expertise.
Specialists can help you navigate insurance denials for CGRP drugs, adjust doses safely, and avoid medication-overuse headaches. They can also check for other conditions-like sleep apnea or TMJ-that might be making your migraines worse.
The Future of Migraine Care
The migraine market is booming. New drugs like atogepant (Qulipta) can be used for both prevention and acute treatment. Non-invasive vagus nerve stimulators are getting smaller and smarter. Wearables are being tested to detect early signs of a migraine-changes in heart rate, skin temperature, or activity-before the pain starts. In five years, we may have personalized treatment plans based on your genes, your habits, and your real-time body data.
But for now, the best approach is simple: treat early, prevent wisely, track everything, and don’t settle for living in pain. Migraine isn’t a life sentence. With the right tools, you can take control.
Can migraine be cured?
There’s no cure for migraine yet, but it can be managed effectively. Many people reduce their attacks by 75% or more with the right combination of prevention, acute treatment, and lifestyle changes. Some even reach a point where they rarely have attacks. Research into gene therapy and neurostimulation is ongoing, and future treatments may offer more lasting relief.
How do I know if I have chronic migraine?
Chronic migraine is diagnosed when you have headaches on 15 or more days per month for at least three months, and at least eight of those days meet the criteria for migraine (pulsating pain, nausea, light/sound sensitivity). If you’re using painkillers more than 10 days a month, you might also be developing medication-overuse headache. A neurologist can confirm the diagnosis using ICHD-3 guidelines.
Are CGRP inhibitors worth the cost?
For people who’ve tried at least three other preventives and still have frequent migraines, yes. CGRP drugs cut headache days by half in over half of users, with fewer side effects than topiramate or beta-blockers. The monthly cost is high-$650-$750-but many manufacturers offer copay assistance programs, and insurance approvals are improving. If your life is severely limited by migraine, the cost may be worth the regained quality of life.
Can I use triptans every day?
No. Triptans should be limited to no more than 10 days per month. Using them more often can cause medication-overuse headache, where your brain becomes dependent and you develop daily headaches. If you’re using them frequently, talk to your doctor about switching to a preventive treatment.
What’s the best way to track my migraines?
Use a digital app like Headache Log or Migraine Buddy. They let you log symptoms, triggers, medications, and sleep patterns in minutes. People who track for 3-6 months identify their personal triggers with 40% more accuracy than those using paper diaries. Knowing your triggers lets you avoid them and plan preventive treatment around high-risk times, like your period or a weather front.
Is Botox effective for everyone?
No. Botox is only FDA-approved for chronic migraine (15+ headache days a month). It’s not for episodic migraine. In clinical trials, it reduced headache days by about 8 per month-better than placebo, but not a miracle. About half of users see meaningful improvement. Side effects are usually mild: neck stiffness or drooping eyelids. It’s a good option if other preventives haven’t worked or caused intolerable side effects.
Can stress cause migraines?
Stress doesn’t cause migraine, but it’s the #1 trigger. Studies show 89% of people link stress to their attacks. It’s often the let-down after stress-like after a big presentation or vacation-that triggers the headache. Managing stress through mindfulness, exercise, or therapy can reduce attack frequency. But you still need medical treatment to stop the neurological process.
Do I need to avoid all trigger foods?
No. Only avoid foods you’ve personally linked to attacks. Common ones include aged cheese, red wine, processed meats with nitrates, MSG, and artificial sweeteners. But many people can eat these without issue. Keeping a diary for 3 months will show you which foods, if any, are your triggers. Eliminating everything unnecessarily can lead to unhealthy eating habits.
What to Do Next
If you’re struggling with frequent migraines, start with a headache diary. Track for three months. Then talk to your doctor. Ask about CGRP inhibitors if you’ve tried at least three older preventives. Consider neuromodulation if you want to avoid daily pills. And if you’re using painkillers more than 10 days a month, don’t wait-get help before it turns into daily headaches. Migraine is treatable. You don’t have to live in pain.
13 Comments
Write a comment
More Articles

Choosing the Right Compression Stockings for Oedema Relief
A step‑by‑step guide to picking the right compression stockings for oedema relief, covering pressure classes, sizing, material, and care tips.
Capecitabine and cancer-related anemia: Strategies for management
In my recent research on cancer-related anemia, I came across some interesting strategies for managing this condition, particularly with the use of Capecitabine. As a chemotherapy drug, Capecitabine has shown promising results in reducing anemia symptoms in cancer patients. One approach includes adjusting the dosage and scheduling of Capecitabine to optimize its effectiveness in treating anemia. Additionally, combining Capecitabine with other treatments, such as iron supplementation, can provide further benefits. It is crucial for cancer patients and their healthcare team to collaborate in finding the most suitable management plan for their specific needs.
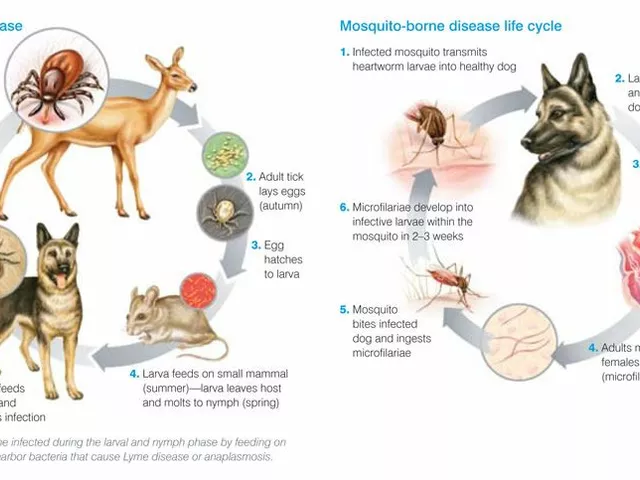
Tick Fever: What You Need to Know About This Dangerous Disease
Tick Fever, also known as Tick-Borne Disease, is a serious illness transmitted by ticks. It's crucial to be aware that this disease can have severe health implications including fever, headache, and fatigue, and in some cases can even be fatal. Early detection and treatment are absolutely vital. It's also important to take steps in preventing tick bites, such as using repellents and wearing appropriate clothing when in tick-infested areas. Stay safe out there, folks!
Vince Nairn
January 7, 2026 AT 02:14I tried topiramate and forgot how to say my own name for three weeks. Then I tried Cefaly and now I can actually watch my kid's soccer games without hiding in the bathroom. No pills. No drama. Just a weird headband that makes my forehead tingle. Worth every penny.
Also, Botox is not a magic wand. I got 31 needles and still had to nap for a week. But hey, at least I didn't die.