Beyond-Use Date: What It Means and Why It Matters for Your Medications
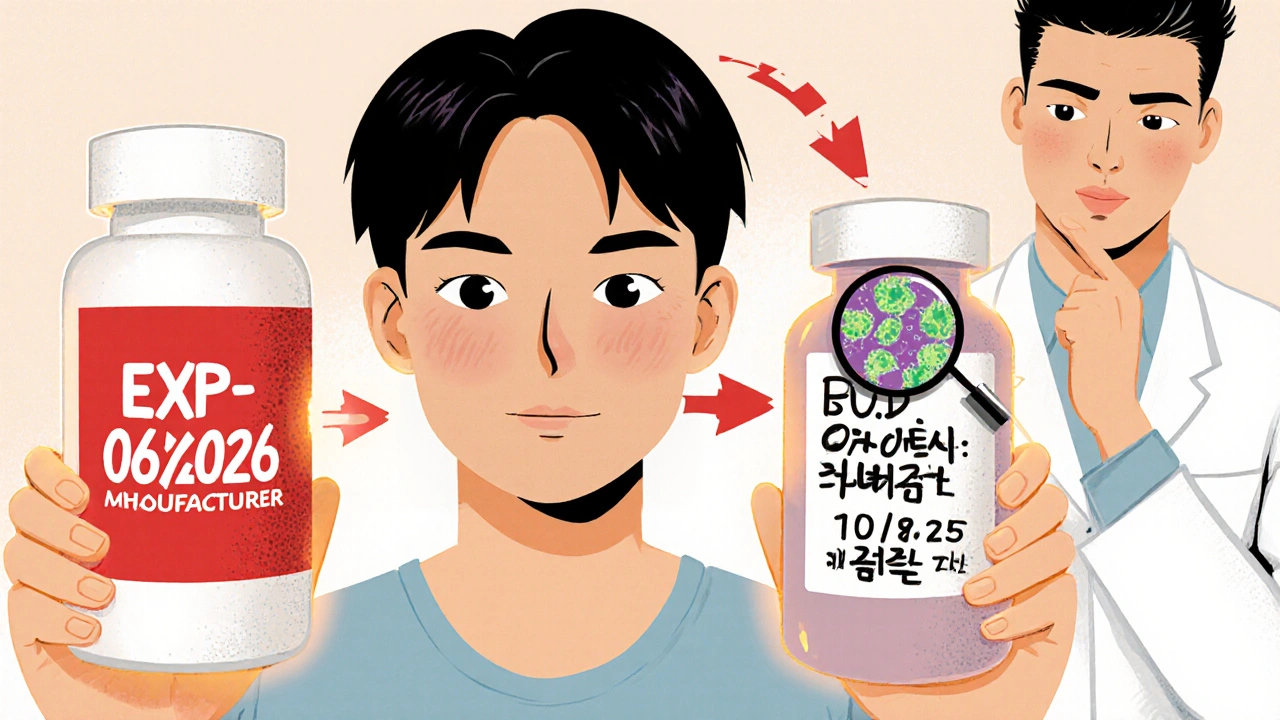
When you pick up a prescription, the label doesn’t always say expiration date—it might say beyond-use date, the date after which a compounded or repackaged medication should no longer be used, set by the pharmacy based on stability data. Also known as beyond-use dating, it’s not the same as the manufacturer’s expiration date, and mixing them up can put your health at risk. This date is handwritten or printed on the label by the pharmacist after they mix, crush, or repackage your medicine. It’s based on science, but also on practical limits—like how long the drug stays stable outside its original container, or how long it lasts once you add liquid to a powder.
Why does this matter? Because medication stability, how long a drug maintains its strength, purity, and safety under specific conditions isn’t guaranteed forever. A pill in its original blister pack might last years. But if your pharmacist puts it in a plastic bottle with a different label, or mixes your antibiotic into a syrup for your child, that stability clock resets. The pharmacy labeling, the official date and instructions printed or written on a repackaged or compounded medication by a licensed pharmacist is your only guide after that point. Ignore it, and you might be taking a weaker dose—or worse, a degraded chemical that could irritate your stomach or trigger an allergic reaction. Studies show that some liquid antibiotics lose potency within weeks after being mixed, even if refrigerated.
And it’s not just about liquids. If your doctor prescribes a custom capsule with three drugs in one, or you get a topical cream from a compounding pharmacy, that beyond-use date is your safety net. It’s set based on real-world testing—not guesswork. Pharmacists consider temperature, light exposure, container material, and even humidity. That’s why you’re told to keep some meds in the fridge and others in a cool, dark cabinet. The same bottle stored wrong might go bad in 14 days instead of 30. And if you’re buying generics or buying online? You can’t assume the beyond-use date is the same as the original box. Always check the label the pharmacy gave you.
You’ll see this in posts about statins, corticosteroids, or even cancer meds—when drugs are repackaged for hospital use or split into smaller doses, the beyond-use date becomes critical. It’s why FDA inspection records look at how pharmacies handle labeling. It’s why pharmacists ask if you’re storing your meds in the bathroom (they know you are). And it’s why some hospitals refuse to use generic cancer combos unless they can prove stability beyond the date on the label.
Bottom line: That little date on your prescription bottle isn’t just bureaucracy. It’s a shield. Take it seriously. Don’t use meds past that date, even if they look fine. Don’t assume they’re still strong. And if you’re unsure? Call your pharmacy. They’re the ones who set it—and they’re the ones who know the science behind it.
Below, you’ll find real-world examples of how beyond-use dates connect to medication safety, compounding practices, and what happens when things go wrong—from statins to chemotherapy to everyday prescriptions. These aren’t theoretical guides. They’re based on what’s happening in pharmacies, hospitals, and patient reports right now.
How to Compare Manufacturer Expiration Dates vs. Pharmacy Beyond-Use Dates
Learn the critical difference between manufacturer expiration dates and pharmacy beyond-use dates for compounded medications. Know when your medicine is safe to use-and when to throw it away.