Candidemia: Understanding the Infection, Risks, and Treatment
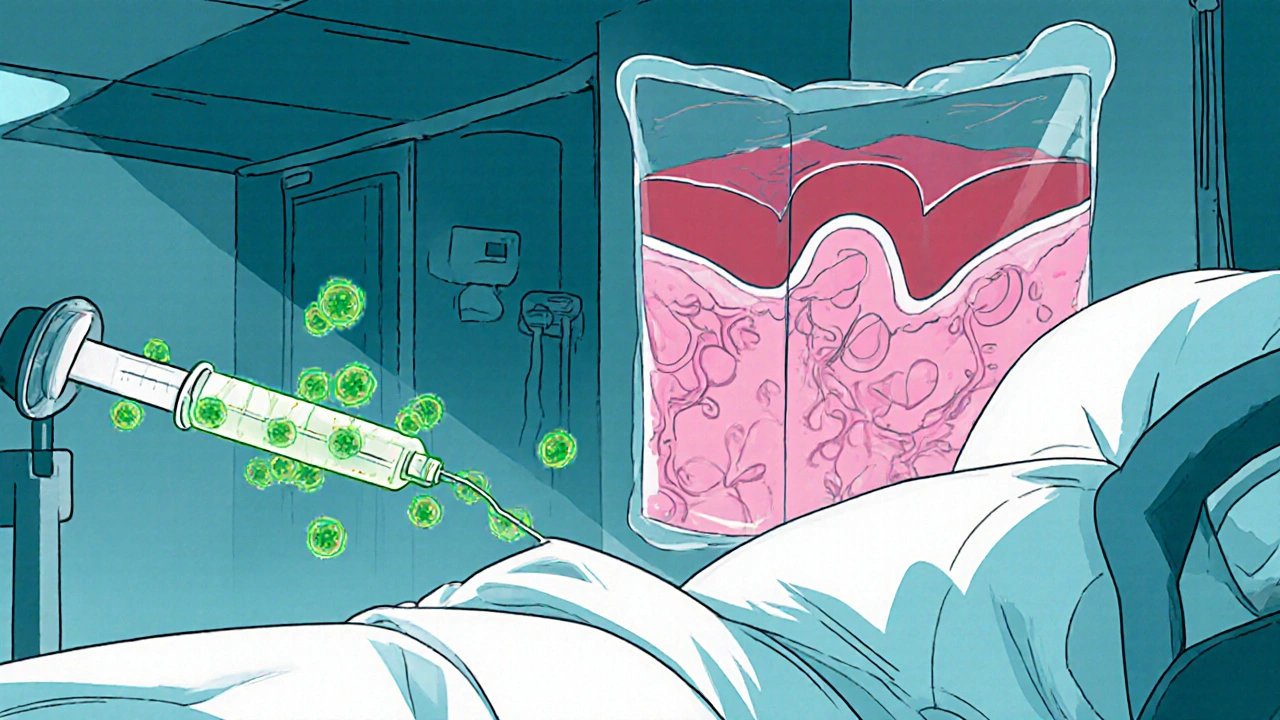
When dealing with Candidemia, a bloodstream infection caused by Candida fungi. Also known as Candida sepsis, it often strikes patients whose immune defenses are weakened, such as those in intensive care units or on long‑term antibiotics. Candidemia can quickly progress to severe sepsis, so early recognition is crucial.
Key Factors in Managing Candidemia
One of the first things to grasp is the role of Candida species, the fungal culprits behind the infection. Over 20 species exist, but C. albicans, C. glabrata, and C. auris account for most cases. These organisms differ in drug susceptibility, making accurate identification a must. The presence of a central line, total parenteral nutrition, or prolonged neutropenia often creates a doorway for these yeasts to enter the bloodstream, linking candidemia to central line‑associated bloodstream infection. Effective treatment hinges on antifungal therapy. Current guidelines favor echinocandins like caspofungin as first‑line agents because they cover most resistant strains, especially C. glabrata. If the isolate is susceptible, a step‑down to fluconazole can shorten hospital stay and lower costs. Timing matters: initiating therapy within 24 hours of positive blood cultures improves survival rates, illustrating the triple relationship that candidemia requires rapid diagnosis, appropriate antifungal choice, and early intervention. Patients with weakened immunity—whether due to chemotherapy, organ transplantation, or HIV—are especially vulnerable. This group, referred to as immunocompromised patients, often display atypical symptoms, making clinical suspicion even more important. In addition to blood cultures, non‑culture tests like serum (1→3)-β‑D‑glucan can flag fungal invasion before cultures turn positive, giving clinicians a head start. Beyond drugs, source control is a non‑negotiable part of care. Removing or replacing infected catheters, draining abscesses, and managing underlying conditions such as uncontrolled diabetes close the loop on infection control. Each step—diagnosis, antifungal selection, and source removal—forms a cohesive chain that keeps candidemia from spiraling into full‑blown septic shock. The articles below dive deeper into each of these areas: from the latest diagnostic tools and risk‑factor breakdowns to step‑by‑step treatment algorithms and patient‑focused management tips. Browse on to equip yourself with practical insights that can help you spot, treat, and prevent candidemia effectively.
Rising Threat of Candidemia and Disseminated Candida Infections in Hospitals
Explore why candidemia and disseminated Candida infections are rising in hospitals, learn to identify at‑risk patients, diagnose quickly, treat effectively, and prevent outbreaks with proven strategies.