Remote Patient Monitoring: How It Works and What It Means for Your Health
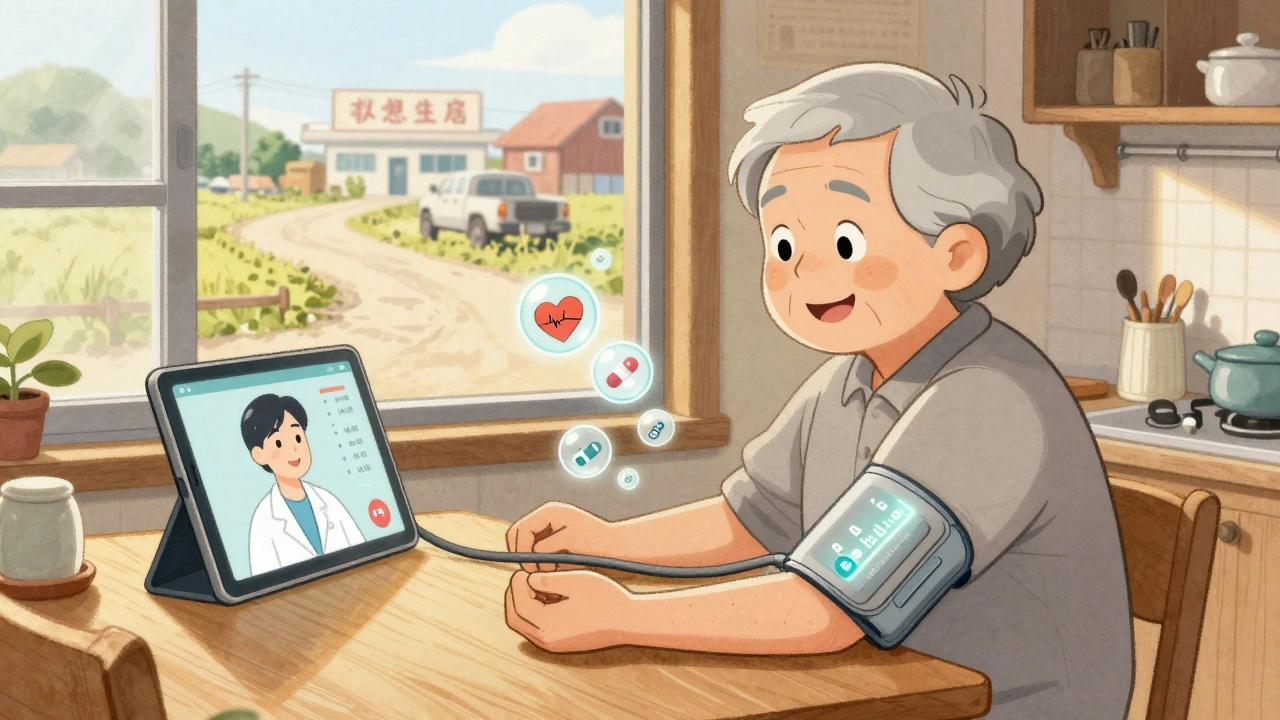
When you think of remote patient monitoring, a system that uses digital tools to track a patient’s health data outside traditional clinical settings. Also known as home health monitoring, it lets doctors see your blood pressure, heart rate, glucose levels, or oxygen saturation in real time—without you leaving your couch. This isn’t science fiction. It’s what millions of people with heart failure, diabetes, or COPD are using right now to avoid ER visits and hospital stays.
It works because of three things: wearable health devices, tools like smart watches, patch sensors, or Bluetooth-enabled scales that collect vital signs, telehealth platforms, secure apps that send data to your care team, and chronic disease management, the structured approach to controlling long-term conditions with consistent tracking. These aren’t separate pieces—they’re connected. Your glucose monitor sends numbers to an app. The app flags a spike. Your nurse gets an alert. You get a call before you feel sick. That’s the whole point.
It’s not just for older adults or people with serious illnesses. Even if you’re managing high blood pressure or recovering from surgery, remote monitoring can catch problems early. One study showed patients with heart failure who used it had 30% fewer hospitalizations. That’s not a guess—it’s data from real people using real devices at home. And it’s not about replacing doctors. It’s about giving them better information so they can act faster, smarter, and before things get dangerous.
You might wonder: Is this safe? What if the device gives wrong numbers? What if I forget to wear it? These are valid questions. The tools aren’t perfect. But the systems behind them are getting better. Many now include alerts for missed readings, automatic calibration checks, and human review when data looks off. It’s not about perfection—it’s about patterns. One high reading? Maybe you had coffee. Five high readings in a week? That’s a signal.
What you’ll find in these articles isn’t marketing fluff. It’s real talk about what works, what doesn’t, and what you need to know before signing up. You’ll learn how to choose a device that actually fits your life, how to handle false alarms without panicking, and why some insurance plans cover these tools while others don’t. You’ll see how people with diabetes, asthma, or after-heart surgery use these systems daily—and how they’ve changed their outcomes.
Telehealth Strategies for Monitoring Side Effects in Rural and Remote Patients
Telehealth is transforming how rural and remote patients manage medication side effects. From smart devices to pharmacist-led monitoring, discover how these strategies reduce hospitalizations and save lives in underserved areas.