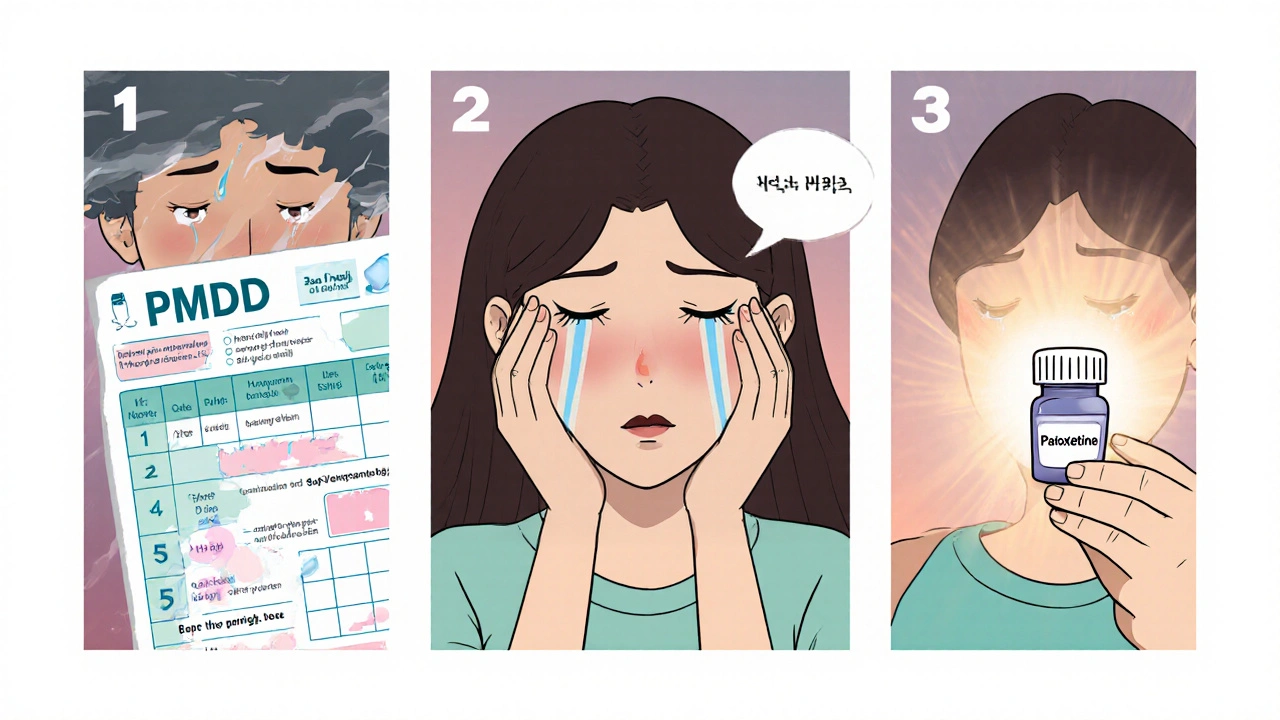
SSRIs for PMDD – Key Facts and Practical Guidance
When dealing with SSRIs for PMDD, the use of selective serotonin reuptake inhibitors to treat premenstrual dysphoric disorder. Also known as antidepressant therapy for PMDD, it offers a proven way to ease severe mood swings before menstruation. The core drug class, Selective serotonin reuptake inhibitor, a medication that boosts brain serotonin by blocking its reabsorption, works by smoothing out the rapid serotonin drops that happen during the luteal phase. SSRIs for PMDD can be taken continuously or only during the symptomatic window, and both strategies have solid research backing them.
How Hormonal Fluctuations Trigger PMDD Symptoms
Understanding the link between the menstrual cycle and mood is crucial. Premenstrual Dysphoric Disorder, a severe form of premenstrual syndrome marked by intense emotional and physical distress rises when estrogen and progesterone swing sharply in the weeks before menses. These hormones affect Serotonin, a neurotransmitter that regulates mood, sleep, and pain perception, lowering its availability and amplifying irritability, anxiety, and depression. The semantic triple here is clear: PMDD symptoms stem from hormonal fluctuations, serotonin modulation mitigates those symptoms, and SSRIs provide the needed serotonin boost.
Another practical point is dosing. Short‑term (5‑day) regimens start a few days before the expected period and stop when bleeding begins, which many women find convenient and less likely to cause side‑effects. Continuous daily dosing, on the other hand, smooths serotonin levels throughout the month and works well for those with lingering mood issues. Studies show that both approaches achieve similar relief, so personal preference, side‑effect profile, and lifestyle dictate the choice.
Side‑effects deserve a quick rundown. Common issues include mild nausea, headache, and temporary sleep changes. Most fade within two weeks, and starting at a low dose often prevents them. If sexual dysfunction appears, adjusting the dose or switching to another SSRI usually helps. The key is open communication with a prescriber – they can fine‑tune the regimen based on real‑world response.
Beyond medication, lifestyle tweaks reinforce the benefits of SSRIs. Regular aerobic exercise boosts natural serotonin, reduces stress, and stabilizes sleep patterns. A balanced diet rich in omega‑3 fatty acids and complex carbs supports hormone balance. Mind‑body techniques such as progressive muscle relaxation or brief meditation sessions can cut the intensity of anxiety spikes during the luteal window.
For those who prefer non‑pharmacological routes, a few studies suggest that calcium supplementation (1,200 mg daily) and vitamin B6 (80 mg) may modestly lessen PMDD severity. However, these measures work best when paired with an SSRI, not as a standalone solution. Combining approaches often produces the most consistent symptom control.
Finally, monitoring is essential. Keep a simple diary noting mood, sleep, appetite, and any side‑effects. Over a couple of cycles you’ll see patterns that help you and your clinician decide whether to stick with the current plan, adjust dosage, or try a different SSRI. The goal is a predictable, manageable cycle rather than a month‑long roller coaster.
Below you’ll find a curated list of articles that dive deeper into each of these topics – from detailed dosing charts to real‑world patient stories, safety tips, and the latest research on serotonin’s role in PMDD. Whatever stage you’re at, the resources ahead aim to give you clear, actionable guidance for a smoother monthly experience.
How Paroxetine Can Help Treat Premenstrual Dysphoric Disorder
Learn how paroxetine, an FDA‑approved SSRI, treats Premenstrual Dysphoric Disorder, including dosage, effectiveness, side‑effects, and comparisons with other therapies.