Types of Glaucoma: How to Spot Each Kind and What to Do
Glaucoma is one of the top causes of irreversible blindness worldwide—and many people don’t notice it until some vision is lost. That’s why knowing the different types of glaucoma matters. Some move slowly and quietly, others strike suddenly and need emergency care. Here’s a clear, no-nonsense rundown so you know what to watch for and how doctors treat each kind.
How each type shows up
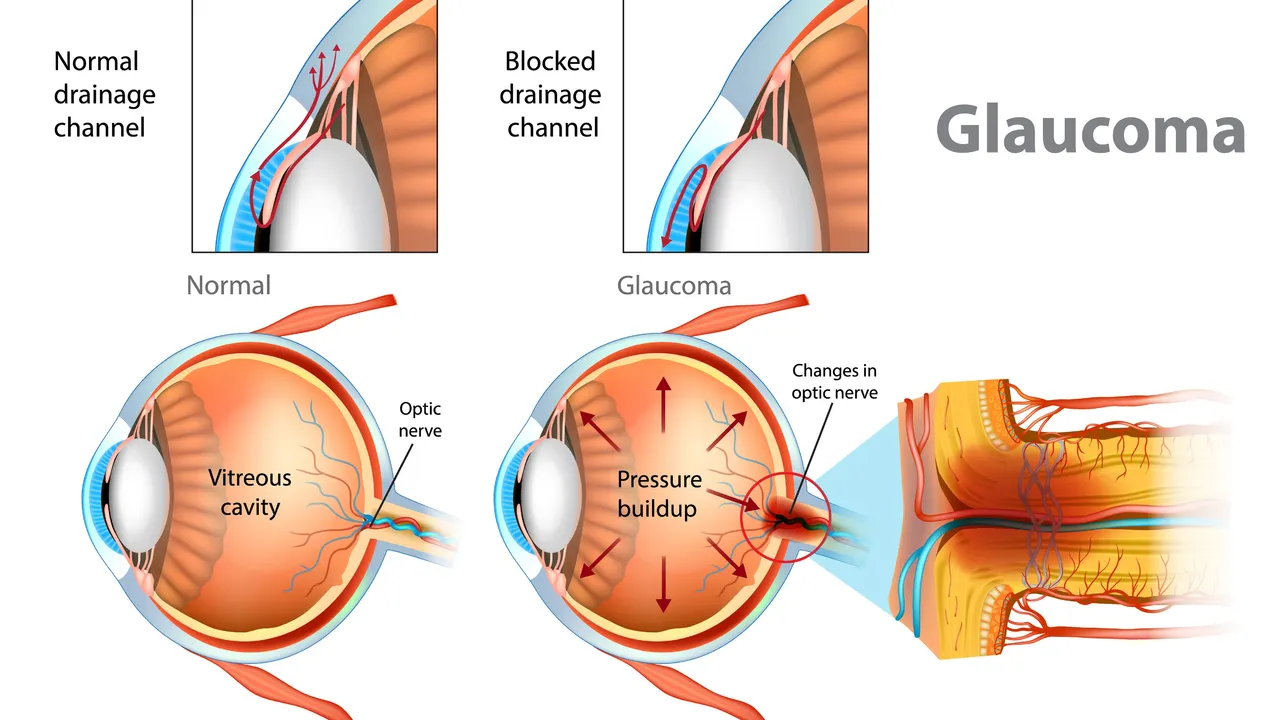
Primary open-angle glaucoma is the most common. The eye’s drainage angle stays open but drainage is inefficient, so pressure rises slowly. Often there are no early symptoms—vision loss starts at the sides and creeps inward. Regular eye checks catch this before major damage.
Angle-closure glaucoma can be an emergency. The drainage angle is blocked, pressure spikes fast. Symptoms: sudden severe eye pain, headache, blurred vision, halos around lights, redness, nausea or vomiting. If you get those signs, go to A&E or an eye clinic right away—delay risks permanent loss.
Normal-tension glaucoma shows optic nerve damage and visual field loss despite eye pressure in the normal range. Doctors suspect blood flow problems or a sensitive optic nerve. It’s diagnosed by careful optic nerve exams and visual field tests.
Congenital glaucoma appears in babies and young children. Look for oversized eyes, cloudy corneas, tearing or light sensitivity. It needs early surgery to protect vision and develop normal sight.
Secondary glaucoma happens because of another condition—eye injury, inflammation, steroid use, advanced cataracts, or new blood vessels after diabetes. Treating the underlying cause is part of the glaucoma plan here.
Diagnosis and treatment: what to expect
Your eye doctor will measure eye pressure (tonometry), check the drainage angle (gonioscopy), examine the optic nerve, and run a visual field test. OCT scans can track nerve fiber loss. Tests help pin down the type and how fast it’s progressing.
Treatment aims to lower pressure and protect the optic nerve. First-line is usually medicated eye drops. If drops aren’t enough, laser options help—trabeculoplasty for open-angle, peripheral iridotomy for angle-closure. Surgery like trabeculectomy or drainage implants is used when other measures fail. For secondary glaucoma, treating the root cause (stopping steroids if possible, managing diabetes) is key.
Want practical tips? Get a full eye exam every 1–2 years if you’re over 40, have family history, are short-sighted, diabetic, or use steroids long-term. If you experience sudden eye pain, halos, severe headache or vomiting with vision change, seek emergency care now. Keep copies of test results and ask your doctor how often to repeat visual field or OCT tests—tracking change early keeps vision safer.
Understanding the types of glaucoma helps you act fast and avoid surprises. Regular checks and quick responses to sudden symptoms are the best defense.
The effectiveness of dorzolamide in treating different types of glaucoma
Hey there, gentlemen! I just wanted to share some insights on a very interesting topic - the effectiveness of dorzolamide in treating different types of glaucoma. We'll dive into its mechanism of action, its beneficial effects on different types of this eye condition, and why it's becoming a go-to medication. Through this, I hope to provide everyone with a deeper understanding of this treatment option in a clear and simple language. Remember, knowledge is your best ally in health matters!