Grapefruit Juice Drug Interactions: What You Need to Know
When you drink grapefruit juice, a common breakfast drink that can dangerously alter how your body processes certain medications. Also known as citrus fruit interaction, it’s not just a myth—it’s a real risk that affects millions who take prescription drugs daily. This isn’t about being allergic or having an upset stomach. It’s about your liver and intestines suddenly losing the ability to break down pills the way they should. The result? Too much drug in your blood—or not enough. Either way, it can land you in the hospital.
The problem isn’t the juice itself. It’s the furanocoumarins in grapefruit that block an enzyme called CYP3A4. This enzyme normally helps break down over 85 medications, including statins, cholesterol-lowering drugs like atorvastatin and simvastatin that can build up to toxic levels when grapefruit is involved, blood pressure meds, like felodipine and nifedipine, where even a small amount of juice can cause your pressure to drop too low, and even some anti-anxiety pills and immunosuppressants. One glass can do it. And the effect lasts up to 72 hours. That means even if you drink grapefruit juice at breakfast and take your pill at night, you’re still at risk.
Not all citrus fruits are the same. Oranges? Safe. Tangerines? Usually fine. But Seville oranges, pomelos, and limes? Avoid them too—they carry the same risk. And don’t think switching to fresh-squeezed or organic helps. The chemicals causing the problem are in the fruit, not the processing. Even a single half-grapefruit can trigger a reaction. If you’re on a long-term medication, especially for heart disease, high cholesterol, or mental health, check your label or ask your pharmacist. Most prescriptions that interact with grapefruit will have a warning on the bottle. If not, don’t guess. A quick call to your pharmacy can save your life.
The good news? You don’t have to give up citrus entirely. Just avoid grapefruit and its close cousins. Swap your morning juice for orange, apple, or cranberry. If you love the taste, try a small amount of lemon in your water. The key is knowing what’s safe and what’s not. This collection of posts dives into real cases, explains which meds are most at risk, and gives you clear steps to avoid dangerous mix-ups—whether you’re on statins, blood pressure pills, or something else entirely. You’ll find practical advice from people who’ve been there, plus expert tips on how to talk to your doctor and read your prescription labels like a pro.
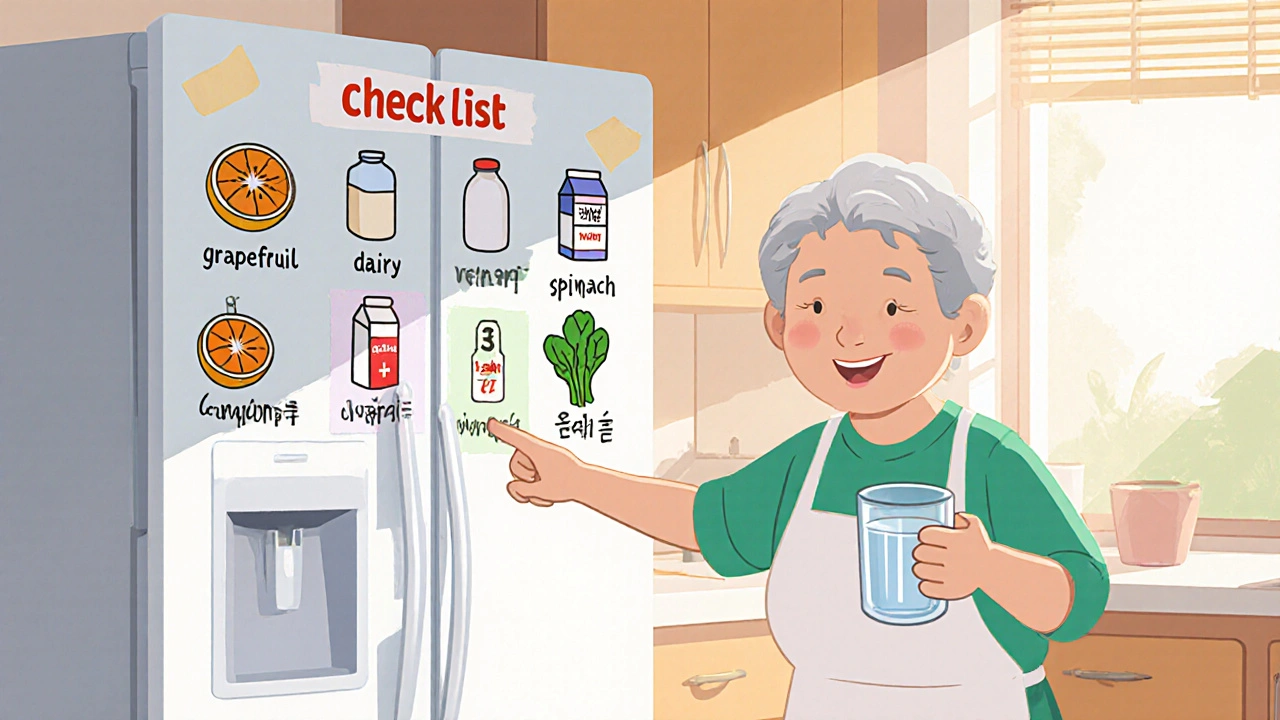
How to Create a Food and Medication Interaction Checklist at Home
Create a simple, personalized food and medication interaction checklist to prevent dangerous reactions. Learn what foods to avoid with common meds like warfarin and statins, how to update it, and where to keep it for maximum safety.