Immunosuppressant Side Effects: What You Need to Know
When your body’s immune system is turned down on purpose, it’s usually because you need it to stop attacking something—like a transplanted organ, a healthy tissue or structure received from a donor that requires medication to prevent rejection. That’s where immunosuppressants, medications designed to reduce immune system activity to prevent rejection or autoimmune damage come in. But turning down your immune system isn’t free. These drugs leave you more vulnerable to infections, raise your risk of certain cancers, and can hurt your kidneys, liver, or blood pressure. They’re life-saving, but they come with trade-offs you need to understand.
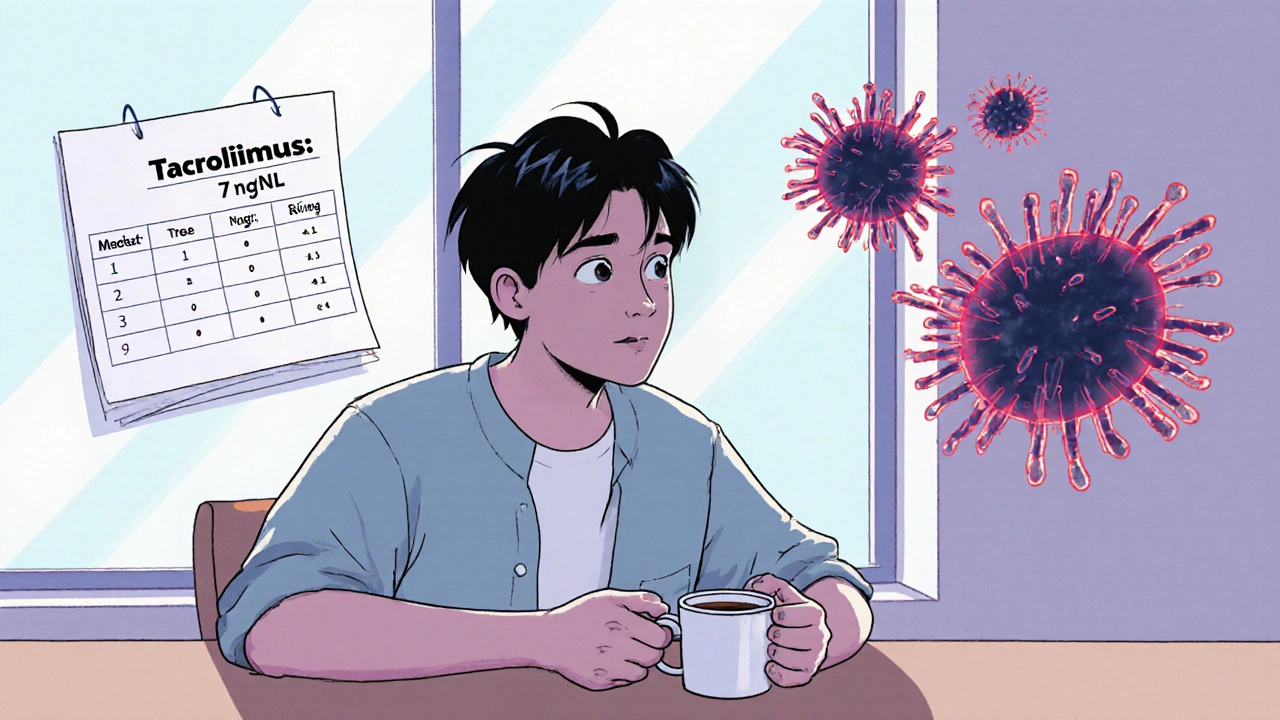
Many people on immunosuppressant side effects don’t realize how common and serious they can be. For example, drugs like tacrolimus or cyclosporine—common after kidney transplant, a surgical procedure replacing a failed kidney with a healthy one from a donor—can cause tremors, headaches, or high blood sugar. Others, like mycophenolate, might lead to nausea or lower white blood cell counts, making even a cold dangerous. And here’s the catch: these drugs don’t work alone. They often mix with systemic antifungals, oral or IV medications used to treat serious fungal infections that can interfere with liver enzymes, like fluconazole or voriconazole. That combo can spike immunosuppressant levels in your blood, leading to toxicity. Even something as simple as grapefruit juice can mess with how your body breaks these drugs down.
It’s not just about the drugs themselves. Your age, other health conditions, and what else you’re taking all play a role. Someone on immunosuppressants after a liver transplant, a surgery replacing a damaged liver with a healthy one might also be on statins for cholesterol, and that’s another potential clash. The same goes for antibiotics, pain meds, or even over-the-counter supplements. Monitoring isn’t optional—it’s daily. Blood tests, tracking symptoms like unexplained fever or fatigue, and knowing when to call your doctor can make the difference between a manageable side effect and a hospital visit.
You’re not alone in this. Thousands of people manage these drugs every day—after transplants, for autoimmune diseases like lupus or Crohn’s, or even for severe eczema. The goal isn’t to scare you, but to arm you. The posts below break down real cases: how one person handled severe nausea from mycophenolate, why a kidney patient had to switch drugs after a fungal infection, and how to spot early signs of infection when your immune system is suppressed. You’ll find practical tips on avoiding dangerous drug combos, what blood tests to ask for, and how to talk to your pharmacist about hidden risks. This isn’t theory. It’s what works for real people trying to stay healthy while their body’s defenses are turned down.
Tacrolimus Neurotoxicity: Understanding Tremor, Headache, and Blood Level Targets
Tacrolimus neurotoxicity causes tremor, headache, and brain fog in 20-40% of transplant patients-even when blood levels are normal. Learn how genetics, electrolytes, and drug interactions affect risk, and what you can do to manage it.