Medication Safety: Protect Yourself from Dangerous Interactions and Side Effects
When you take a pill, you're not just dealing with one substance—you're entering a hidden world of chemical reactions inside your body. Medication safety, the practice of using drugs in a way that minimizes harm while maximizing benefit. Also known as drug safety, it's not about following labels blindly—it's about understanding what your meds are really doing to you. Every year, hundreds of thousands of people end up in the ER because of avoidable mistakes: mixing statins with grapefruit juice, taking expired antibiotics, or not realizing that a common antacid can cancel out your heart medication. This isn't fear-mongering—it's fact. The FDA reports that over 1.3 million emergency visits each year are tied to medication errors, and most of them happen at home.
Drug interactions, when two or more medications react in a way that changes their effect. Also known as pharmacological interactions, it's the silent killer in plain sight. Think of it like a traffic jam inside your liver. Some drugs slow down how your body breaks down others, letting them build up to toxic levels. That’s why systemic antifungals can turn your statin into a muscle-destroying bomb, or why warfarin turns harmless leafy greens into a bleeding risk. Then there’s adverse drug reactions, unexpected side effects that aren’t listed because they’re rare or delayed. Also known as ADR, these are why someone on prednisone suddenly gets brittle bones, or why a daily atorvastatin leads to unexplained fatigue or erectile dysfunction. These aren’t rare flukes—they’re predictable if you know where to look. And don’t forget steroid side effects, the long-term damage from daily corticosteroid use that many patients never connect to their meds. Also known as chronic steroid toxicity, this includes thinning skin, high blood sugar, and even adrenal shutdown when you try to stop. These aren’t just side effects—they’re slow-motion health crises.
Medication safety also means knowing when your pill is no longer safe. Expired medication, anything past its manufacturer or pharmacy-determined use-by date. Also known as beyond-use date, it’s not just about potency—some drugs degrade into toxins. Compounded meds, cancer drugs, and even common antibiotics can become dangerous after their labeled date. And here’s the kicker: pharmacies often set their own expiration dates that are shorter than the manufacturer’s. Most people don’t know the difference—and that’s how you end up taking a weak or toxic dose.
What you’ll find below isn’t a list of warnings—it’s a practical toolkit. Real stories. Real science. Real fixes. From how to build a food-and-drug checklist that actually works, to why your asthma inhaler might be giving you thrush, to how to spot when a generic cancer drug could be putting you at risk. No fluff. No theory. Just what you need to keep yourself and your loved ones safe—day after day, pill after pill.
How to Use Patient Counseling to Catch Dispensing Mistakes in Community Pharmacies
Patient counseling catches 83% of dispensing errors before they reach patients-more than barcode scans or double-checks. Learn how asking the right questions, checking pill appearance, and using teach-back methods can prevent deadly mistakes in community pharmacies.
How to Read Directions for Extended-Release Medications on Labels
Learn how to safely read and follow instructions on extended-release medication labels to avoid dangerous mistakes like crushing pills or taking them at the wrong time. Understand ER, XR, SR, and CR labels and why timing matters.
Barcode Scanning in Pharmacies: How It Prevents Dispensing Errors
Barcode scanning in pharmacies prevents up to 93% of medication errors by verifying the right patient, drug, dose, route, and time. Learn how this technology works, where it fails, and why it’s essential for patient safety.
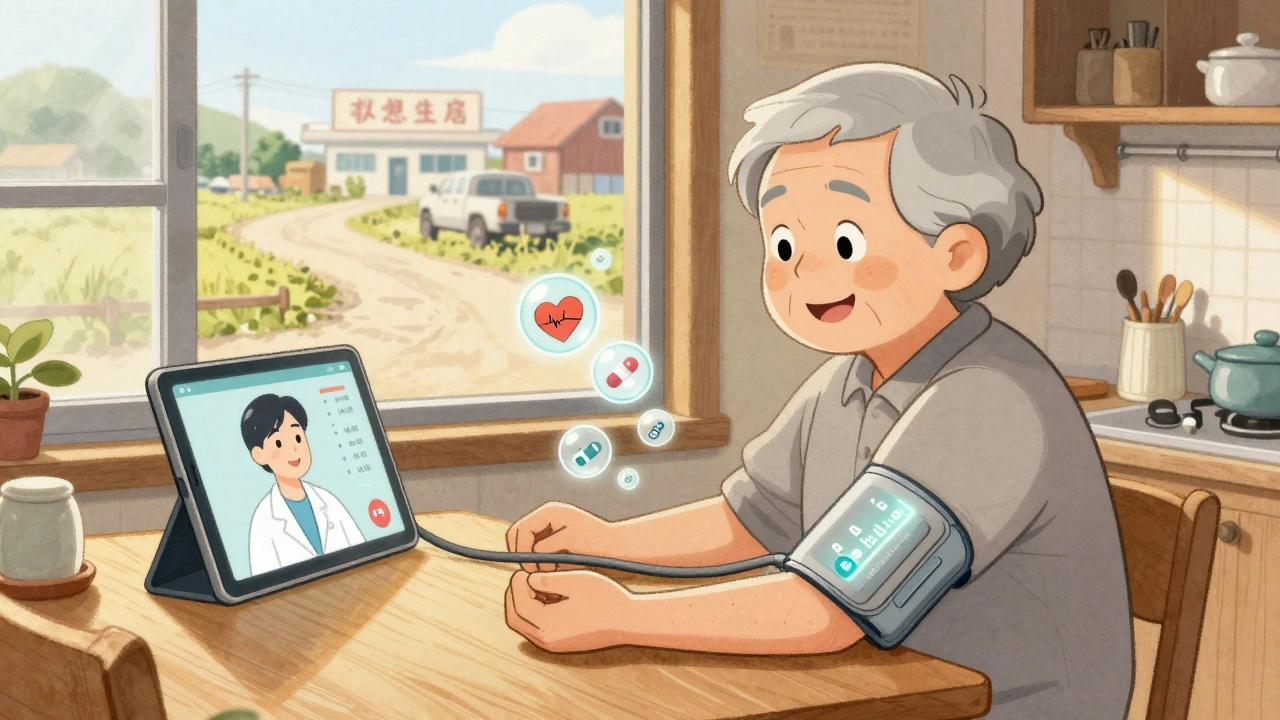
Telehealth Strategies for Monitoring Side Effects in Rural and Remote Patients
Telehealth is transforming how rural and remote patients manage medication side effects. From smart devices to pharmacist-led monitoring, discover how these strategies reduce hospitalizations and save lives in underserved areas.
Poison Control Hotline: How It Works and What to Report About Medications
Learn how the poison control hotline works, what details to report about medications, and why calling 1-800-222-1222 can prevent ER visits and save lives. Free, expert help 24/7.
Post-Menopausal Women and Medication Changes: Safety Considerations
Post-menopausal women face unique medication risks due to hormonal shifts, polypharmacy, and age-related changes. Learn how to safely manage hormone therapy, avoid dangerous drug interactions, and reduce medication errors with practical, evidence-based strategies.
Patient Safety Goals in Medication Dispensing and Pharmacy Practice: How to Prevent Errors and Save Lives
Discover the real-world safety goals that prevent medication errors in pharmacies and hospitals. Learn how barcode scanning, high-alert drug controls, and system redesign-not just training-save lives.